Sanuvox Technologies founder Normand Brais explains why UV purification is the most effective air disinfection method for medical, commercial and residential environments.
Evidence has accumulated over the years that following the standard guidelines and codes for designing healthcare facility ventilation systems is far from sufficient to ensure a sterile environment1-4. Sterility is generally defined as 6 log (99.9999%) reduction of a population of microorganisms. This means that as little as one microorganism in a million is expected to survive after disinfection.
Traditional air filtration with high-efficiency particulate air (HEPA) filters or ultra-low penetration air (ULPA) filters have been widely adopted in the ventilation systems of hospitals, labs, and clinics, to control airborne pathogens. However, multiple studies have demonstrated that despite the use of such high-end filters, viral and bacterial airborne contamination are still ubiquitous in these ventilation systems5-7.
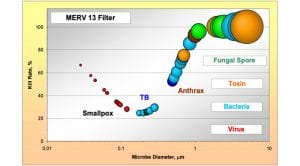
The most common explanation for underperforming filters often points to the filter rack seal joint’s bypass, filter puncture leakage, and poor general installation or maintenance. Although all these points remain valid and can always be improved, the physical cause is rooted in the fundamental fact that all filters show a significant drop in their capture efficiency for a certain range of particulate sizes – these can include both particles which are too small to be captured by interception and impaction and those which are too large to be removed via electrostatic and diffusion. This is simply a straightforward consequence of the fundamental principles of filtration physics8.
HEPA filters are no different and display a weakness at a critical particle size between 0.1 and 0.4 microns, as shown in Fig. 1. The HEPA filter efficiency drops to a value just shy of 99.95% at a critical point called MPP (Most Penetrating Particle) which is around 0.2 microns.
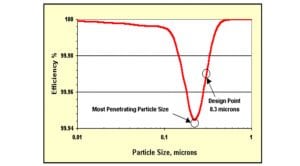
When a concentration of one million particles fall within the vulnerable size range for a HEPA filter, for instance, as many as 500 particles of air will pass through the filter. During a single day, a small flow of 1,000m3 per hour of ‘fresh outside air’ from the ventilation system could allow up to 12 million microorganisms to contaminate the aseptic zone.
Table 1 shows in red a list of microorganisms which are difficult to capture by HEPA filters. Medical specialists and microbiologists will easily recognise that many of the listed bio-contaminants are undesirable in a medical environment.

Table 1 shows that, when challenged by one million particles, some viable microorganisms are able to penetrate through the filter. Considering that sterility is defined as less than one survivor for a million-microorganism population, it is quite clear that the air disinfection process by filtration alone is not sufficient and requires an additional step.
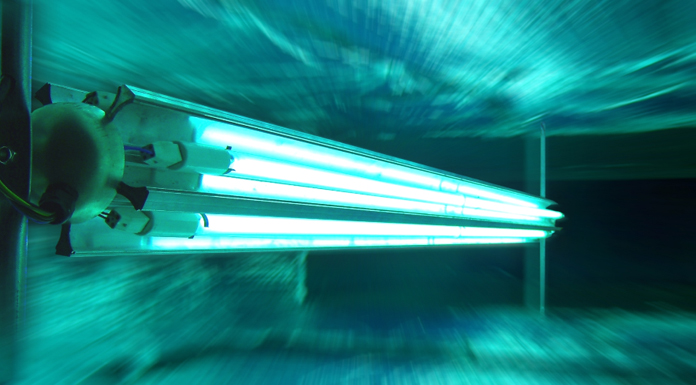
Unlike filtration, ultraviolet germicidal irradiation (UVGI) does not capture or retain microorganisms; it sterilises them by damaging their DNA/RNA strands as they pass through an intense germicidal UV light zone. Unlike filters that accumulate dust until the pressure drop increases to a point where it needs replacement, a UV air disinfection system causes no pressure drop and requires comparatively very low maintenance.
How does UV disinfection work?
The UV light spectrum
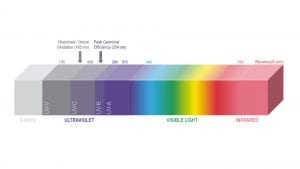
Being outside our visible range, the UV light spectrum, which extends from 100nm to 400nm, is not visible to the human eye. The overall UV spectrum has been subdivided into four bands:
- UVA band (400nm to 315nm): the most abundant in sunlight reaching the Earth’s surface;
- UVB band (315nm to 280nm): primarily responsible for sunburn;
- UVC band (280nm to 200nm): the most effective for germicidal effect; and
- Far or Vacuum UV (200nm to 100nm): ozone generation.
UV disruption of DNA and RNA explained
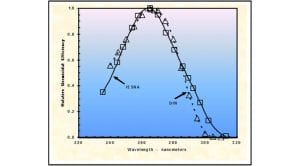
The discovery of microbial disinfection by UV light dates back to 18779. Subsequently, in 1928 FL Gates10 identified the specific wavelength of UV light that was responsible for the observed germicidal effect. Recent biochemical research has shown that the most effective germicidal wavelength of 265nm coincides with the peak absorption spectra of nucleic acids11. Based on this correlation, most of the damage inflicted on sterilised microbes were found in their genetic material.
The primary recognised mechanism in UV disinfection is now confirmed to be cumulative molecular damage to DNA and RNA strands. The disruption of nucleic acids by UV light can affect the complete spectrum of microorganisms, making them sterile when given a sufficient dosage, and consequently unable to infect a host. Within the limits of experimental accuracy, the lethal action of germicidal UV appears to be independent of the nature of the organism and, unlike antibiotics, there has been no signs of adaptive resistance after more than fifty years of UV water disinfection.
Most, if not all, commercially available germicidal light sources are based on fluorescent tube technology and emit between 30% and 35% of their input power at 253.7nm, a wavelength very close to the peak germicidal wavelength of 265nm as shown in Fig. 3. In comparison, current LED technology has only 4% to 6% efficiency when it comes to UVC emission.
UVGI sterilisation of microorganisms is therefore achieved in practice with the low-cost and widely available wavelength of 253.7nm. The quantum energy carried by these photons is high enough to disrupt most single chemical bonds between carbon, hydrogen, oxygen and nitrogen atoms. The molecular reactions caused by these energetic photons result in irreversibly damaging the nucleic acids of a microorganism until it is no longer viable.
Amongst various UV radiation damages to DNA, the formation of cyclobutene pyrimidine dimers (CPDs) and pyrimidine-pyrimidine four to six photoproducts (PPs)12, CPDs are caused by covalent bonding between two adjacent pyrimidines. However, as shown in Fig. 4, UVC usually generates thymine dimers in the greatest quantity, cytosine dimers in low quantity and mixed dimers at an intermediate level. In UV-irradiated RNA viruses, the nucleotide uracil forms pyrimidine photoproducts. At an irradiation dose of magnitude high enough to overwhelm the nucleic acid repair mechanisms, damages result in irreversible alterations, impairment of replication and genetic transcription, and eventual death of the organism.
For a thorough assessment of the photochemistry of UV-induced damages to nucleic acids, and on repair mechanisms, review the in-depth description by Kowalski13.
UVGI dosage required to complete air sterilisation
Given a known UVGI intensity in milliwatts per square centimetre and exposure time in seconds, the product of which is called the ‘UV dose’ expressed in millijoules per square centimetre, there is a direct mathematical relation that predicts the disinfection rate for each microorganism.
Let us review the list of the microorganisms of concern shown in Table 2 that fall within the vulnerable size range of HEPA filters and look at their reduction with the addition of a UV dose.
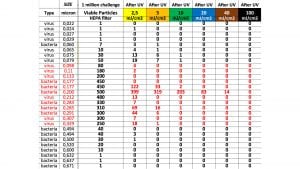
The baseline UV dose for disinfection of the air in offices and commercial buildings is 2.5mJ/cm2. It is what we call a yellow belt level. As the UV dose is progressively increased and reaches 100mJ/cm2, the air is deemed sterile.
This UV dosage ensures an overall disinfection of at least 99.9999% for all of the microorganisms of concern, including the most filter-penetrating and UV-resilient microorganism Francisella Tularensis.
Repeating the above exercise, but with a higher performing ULPA filter, where the efficiency is equal or greater than 99.99%, the UV dose needed to complete the disinfection to obtain 6 log air sterility drops to 40mJ/cm2.
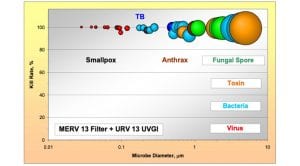
Because it is practically impossible to upgrade from regular filters (MERV 8 to MERV 13) to high HEPA or ULPA filters most of the time, due to excessive pressure drop that would choke the air flow, it is interesting to consider the optimum balance between filtration and UVGI.
The combination of MERV 13 with UV provides the best overall air disinfection performance while minimising energy operating cost.
Fig. 5 shows that despite the low efficiency of MERV 13 filter for certain particulate sizes, the addition of UVGI can easily compensate to bring the overall efficiency to a similar level to that of the HEPA filter.
The correct calculation for predicting the applied UV dose must consider the relevant input parameters describing a UVGI system in terms of its geometry, lamp characteristics, lamp placement, lamp orientation, and surface reflectivity. The program requires the following input parameters for each computation:
- Airflow rate;
- Height, width, and length of duct;
- Percentage reflectivity of inner surfaces;
- UV lamp length, diameter and output power;
- 3D positioning co-ordinates of each lamp; and
- Target microorganisms’ UV susceptibility values.
The efficiency of germicidal UV in air disinfection
When properly engineered, germicidal ultraviolet systems can efficiently complete the air disinfection initiated by HEPA filters. UVGI is a predictable, low-cost, reliable and mature technology for eliminating pathogens. Public health agencies such as the US Centers for Disease Control and Prevention (CDC) recommend the use of UVGI to disrupt the transmission of pathogens in buildings’ ventilation systems.
The relative rarity of UV disinfection is predominantly due to the false perception that HEPA air filters are sufficient to provide sterilised air. Years of accumulated field experience have shown that filters are certainly necessary but not sufficient. When dealing with sub-micron biocontaminants in the size range of 0.1 to 0.4 microns – including the infamous SARS-CoV-2 virus – even the best filtration technologies fail. Unlike filters, UVGI technology does not capture microorganisms but it can effectively deactivate them when a proper dosage of ultraviolet energy is applied.
About the author
Normand Brais holds a mechanical engineering degree, a master’s degree in applied sciences, and a doctorate in nuclear engineering from Polytechnique University of Montreal. He was appointed Professor at the Energy Engineering Institute after he graduated.
He has founded several technology companies in various fields such as air pollutants from combustion equipment, biomass combustion, photonics, and ultraviolet disinfection. In 1995 he founded Sanuvox Technologies, which is now a worldwide leader in UV disinfection technology for hospitals, labs, and commercial buildings.
References
1 American Institute of Architects. Guidelines for design and construction of hospital and healthcare facilities. AIA, 2001.
2 American Society of Heating, Refrigerating, and Air-Conditioning Engineers. HVAC Design Manual for Hospital and Clinics. ASHRAE, 2003.
3 Ibid. Handbook – HVAC Applications. ASHRAE, 2003.
4 CDC. Guidelines for Environmental Infection Control in Healthcare Facilities. US Department of Health and Human Services/Centers for Disease Control and Prevention, 2003.
5 Shinsuke K, Minki S. (2011). Using UVGI to counter contaminant dispersion. IFHE Digest.
6 Menzies D, Popa J, Hanley JA, Rand T, Milton DK. Effect of ultraviolet germicidal ligths installed in office ventilation systems on workers’ health and well being: double-blind multiple cross-over trial. The Lancet Medical Journal, 2003. pp. 1785-91. Vol. 362.
7 Menzies D, Adhikari N, Arietta M, Loo V. Efficacy of environmental measures in reducing potentially infectious bioaerosols during sputum induction. Infection Control and Hospital Epidemiology, 2003, Vol. 24.
8 Kowalski WJ, Bahnfleth W. MERV Filter Models for Aerobiological Applications. Air Media. Summer 13-17, 2002.
9 Downes A, Blunt T. Research on the effect of light upon bacteria and other organisms. Proceedings of the Royal Society, 1877. 26:488.
10 Gates FL. On nuclear derivatives and the lethal action of UV light. Science, 1928.
11 Davidson JN. The biochemistry of nucleic acids. Methuen, 5th edition, 1965.
12 Setlow RB. Cyclobutane-type pyrimidine dimmers in polynucleotudes. Science. 1966, Vol. 153: 379-386.
13 Kowalski WJ. Ultraviolet Germicidal Irradiation Handbook. Springer-Verlag, 2009.
14 Kowalski WJ, Bahnfleth WP, Hernandez MT. (Conference paper, 2019). A genomic model for the prediction of Ultraviolet inactivation rate constants for RNA and DNA viruses.
15 Luckiesh M, Holladay LL. Designing installations of germicidal lamps for occupied rooms. General Electric Review, 1942. Vol. 45(6), 343-349.
16 Kowalski WJ. Design and optimisation of UVGI air disinfection systems. A thesis in Architectural Engineering. Penn State, 2001.
17 Lee B, Bahnfleth W, Auer K. (Conference paper, 2019). Life cycle cost simulation of in-duct ultraviolet germicidal irradiation system.
18 Kowalski W. Hospital Airborne Infection Control. Taylor & Francis, 2012. 978-1-4398-2196-1.
19 American Society of Heating, Refrigerating and Air Conditioning. ASHRAE Handbook Chapter 16. ASHRAE, 2008.
This article is from issue 17 of Health Europa. Click here to get your free subscription today.
























