The past few years saw significant progress in the osteoporosis management landscape, but are all patients feeling the benefit?
The introduction of the Fracture Liaison Services (FLS) in the United Kingdom in the late 1990s1 is recognised as a progressive milestone in the management of osteoporosis and fragility fractures and remains a profound example of what good looks like in coordination of care among multiple disconnected players.
At inception, the service sought to address the growing problem of osteoporosis and fragility fractures while also addressing challenges in the management of these patients. 2 Fast forward 20 years and the International Osteoporosis Foundation (IOF) have recorded 388 FLS in over 35 countries, and the benefit of these systems is widely acknowledged: studies have shown that the FLS model, not only reduces the frequency of subsequent fractures and improves adherence to treatment, it also provides cost savings. 3,4,5,6 The IOF go so far as to say that: “The implementation of FLS is the single most important thing that can be done to directly improve patient care and reduce spiralling fracture-related healthcare costs worldwide”. 7
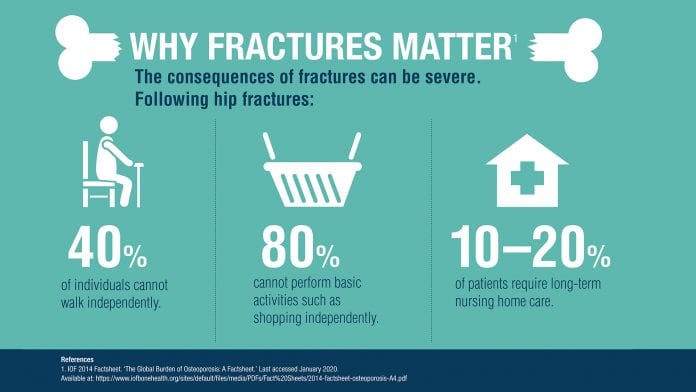
Yet despite this progress and commitment, issues and challenges remain. Osteoporosis is estimated to affect 200 million people worldwide8 and is the most common bone disease in the world, resulting in more than 8.9 million fragility fractures each year around the globe. 9 A sizeable hurdle in tackling fragility fractures is patient perception: data shows that most patients who have sustained a fragility fracture do not recognise that weakened bones are the cause. Instead, there is a common misconception on the patient’s part that fractures are caused by hazards in the environment, random events or are an inevitable part of ageing. 10,11,12,13
This lack of patient awareness and action is coupled with a lack of healthcare professional (HCP) awareness and intervention. Despite women aged 60 and over being most at risk of osteoporosis and fragility fractures, a survey by UCB (of women aged over of 60) found that 37% claimed their HCP had never spoken to them about these issues.14 If these patients aren’t appropriately referred to a FLS or secondary care setting after a fracture, these patients will fall into the ‘osteoporosis treatment gap’.
The issue is set to only get worse with time: between 2015 and 2030, the number of people in the world aged 60 years or over is projected to grow by 56%, from 901m to 1.4bn, and by 2050, the global population of older people is projected to more than double its 2015 size, reaching nearly 2.1bn.15 More needs to be done to ensure a global ageing population have access to the care they deserve.
While the FLS have made progress in addressing the treatment gap, notable discrepancies remain in the level of care for patients. In some cases, patients with fragility fractures who seek medical attention do not receive the appropriate bone health assessment or treatment. 16
The impact of osteoporosis and fragility fractures on individuals and healthcare systems is larger than people realise. Patients and HCPs alike can play a role in tackling this growing issue. Greater public awareness of fragility fractures and their risk factors and warning signs will go some way to raising these issues to national and global discussion. As we approach the 20th anniversary of the FLS, it’s time to reflect on the achievements made to date but also to reinvigorate our collective commitment to patients, helping to protect them from future fractures and so make their first fracture, their last fracture.
This article has been written by Brandon Drew, Vice President at UCB Inc. UCB Pharma SA has full editorial oversight and control.
 Brandon Drew, Vice President & Global Head of Bone
Brandon Drew, Vice President & Global Head of Bone
Immunology Solutions at UCB Pharma SA
Email: brandon.drew@ucb.com
References
- McLellan AR et al. The Fracture Liaison Service: success of a program for the evaluation and management of patients with osteoporotic fracture. Osteoporosis Int. 2003;14(12):1028–34.
- IOF Capture the Fracture. Available at: https://www.capturethefracture.org/map-of-best-practice. Last accessed January 2020.
- Boudou L, Gerbay B, Chopin F, et al. Osteoporos Int. 2011;22(7):2099–106. (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6140089/#b9-ms114_p0295). Last accessed August 2019.
- Marsh D, Akesson K, Beaton DE, et al. IOF CSA Fracture Working Group. Osteoporos Int. 2011; 22(7):2051–65.
- McLellan AR, Wolowacz SE, Zimovetz EA, et al. Osteoporos Int. 2011;22(7):2083–98.
- Nakayama A, Major G, Holliday E, et al. Osteoporos Int. 2016;27(3):873–879.
- IOF Capture the Fracture. Available at: https://www.capturethefracture.org/about. Last accessed August 2019.
- Reginster JY, Burlet N. Osteoporosis: A still increasing prevalence. Bone. 2006;38(2 Suppl 1):S4–9.
- Ström O, Borgström F, Kanis JA, et al. Osteoporosis: burden, health care provision and opportunities in the EU: a report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA). Arch Osteoporos. 2011;6:59–155. doi: 10.1007/s11657-011-0060-1.
- AlamI S, et al. Barriers to Effective Postmenopausal Osteoporosis Treatment: A Qualitative Study of Patients’ and Practitioners’ Views. PlosOne. 2016;11:e0158365.
- Besser SJ, et al. How do osteoporosis patients perceive their illness and treatment? Implications for clinical practice. Arch Osteoporos. 2012;7:115–24.
- Barker KL, et al. A qualitative systematic review of patients’ experience of osteoporosis using meta-ethnography. Arch Osteoporos. 2016;11:33.
- Giangregorio L, et al. Osteoporosis risk perceptions among patients who have sustained a fragility fracture. Patient Education and Counselling. 2009;74:213–20.
- Harris Interactive. Osteoporosis and Fragility Fracture Risk Survey 2018.
- International Osteoporosis Foundation. IOF Compendium of Osteoporosis – First Edition. Last accessed April 2018.
- Walters S, et al. (2017). Fracture liaison services: improving outcomes for patients with osteoporosis. (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5237590/). Last accessed September 2019.

























