Emerging research shows traditional disinfectants may not be able to wipe out antibiotic-resistant organisms.
On any given day, one in 18 patients in a European hospital has a healthcare-associated infection1. Emerging research, looking at why some outbreaks seem impossible to resolve, shows that dry surface biofilms are present on up to 95% of ‘disinfected’ surfaces.
An ICU within one of Australia’s top tertiary care hospitals is decommissioned2. ICUs frequently house immunocompromised patients undergoing multiple invasive interventions, making good infection prevention critical to their outcomes. Effective surface disinfection is a vital step in preventing the spread of healthcare-associated infections (HCAIs).
Once the ward is shut down, it undergoes two rounds of deep cleaning and disinfection with chlorine-based disinfectant. According to laboratory tests, chlorine should be effective against microbes such as MRSA and VRE, common antibiotic-resistant organisms that cause HCAIs. However, when researchers begin taking samples from the environment, they notice something unusual. Despite being twice disinfected with chlorine, researchers find more than half of the surfaces still grow multi-drug resistant organisms3.
To understand how pathogens had survived the chlorine, researchers cut samples from the surfaces themselves. When examined under electron microscopy, they found evidence of dry biofilms on 93% of surfaces3.
Dry surface biofilms – the hidden cause of persistent outbreaks?
Traditionally, we tend to think of microorganisms as free-floating. Most disinfectant efficacy testing is done on these ‘planktonic’ free-floating organisms. Unfortunately, this is not always how microbes behave in the real world.
When microbes attach to a surface, they can form protective biofilms. Different microbial species work together to construct a protective matrix that traditional disinfectants cannot penetrate4–6. With multiple species sheltering within the same biofilm, microorganisms can pass antibiotic resistance genes from one species to another. When we allow biofilms to form, microbes become much harder to kill, both with disinfectants and antibiotics.
For a long time, focus on biofilms was limited to ‘wet’ environments (often sinks or drains). But the outbreak in Australia was not traced back to a sink or drain. It highlighted a role for ‘dry’ biofilms within an outbreak.
How common are dry surface biofilms?
That is what a group of researchers in the UK set out to understand. There is currently no standard test to detect dry surface biofilms, so the team conducted a multi-centre study, sampling everyday items from three hospitals in the UK. Each of the items had already been terminally disinfected.
When swabbed using traditional microbiological techniques, none of the items grew viable organisms. On the surface, it appeared that the traditional disinfectants had done their job. However, when the researchers placed cut pieces from each item into a nutrient broth, viable dry surface biofilms were found on 95% (60/61) of terminally disinfected healthcare items5. More than half of those samples grew antibiotic-resistant microorganisms.
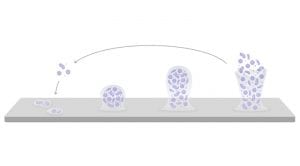
The work from the UK suggests that, whilst traditional disinfectants had killed the free-floating microorganisms, the dry surface biofilm provided a ‘life raft’, allowing the microbes to quickly re-establish themselves.
Despite being based at opposite ends of the Earth, the work from the UK and Australian groups paints a consistent picture. Dry surface biofilms appear far more common than previously thought; our current surveillance techniques cannot detect their presence; and traditional disinfectants allow the biofilms to recover quickly.
How do we wipe out dry surface biofilms?
After discovering dry surface biofilms are virtually universal on healthcare surfaces, researchers at Cardiff University in the UK began extending their investigation, asking the question: why had regular disinfection with sodium hypochlorite not worked in those international outbreaks7?
Often, when assessing disinfectants, we look at one key measure: log reduction. That tells us how many viable microbes a disinfectant can inactivate. When researchers tested various chlorine-based formulations, they found most could not produce a high enough log reduction to eradicate the biofilm.
One formulation did produce a high log reduction: sodium hypochlorite. However, researchers found that, after treatment with sodium hypochlorite, the biofilm became highly transferable7. The hypochlorite had ‘opened’ the biofilm, allowing it to seed microbes into the environment.
Those findings are not surprising. Organic matter inactivates chlorine-based disinfectants8 and biofilm matrices are mainly composed of organic matter. Equally, chlorine-based disinfectants readily transfer hard-to-kill organisms into the environment9.
Searching for an effective way to combat dry surface biofilms, the researchers turned to an alternative disinfectant frequently shown to outperform chlorine: peracetic acid.

Peracetic acid-generating technology
Peracetic acid is a powerful oxidative disinfectant. Unlike chlorine, it is not inactivated by organic matter, making it a great candidate for tackling dry surface biofilms. The biggest challenge is stability: peracetic acid has a short shelf life unless kept at a very low pH. Many generic peracetic acid formulations are highly acidic and corrosive.
Clinell Peracetic Acid Wipes use patented technology to overcome those limitations. Rather than relying on keeping liquid peracetic acid at a low pH, Clinell Peracetic Acid Wipes only generate active ingredients when exposed to water immediately before use. That means they work at a near-neutral pH to help prevent damage to surfaces.
Investigators at Cardiff University tested common healthcare disinfectants against dry surface biofilms. They found that Clinell Peracetic Acid Wipes produced the highest reduction in viable organisms. Clinell Peracetic Acid Wipes were the only disinfectant to completely prevent the biofilm from transferring to other surfaces and delayed regrowth of the biofilm for 6.5 days7.
Formulation is key
Clinell Peracetic Acid Wipes (formerly known as Clinell Sporicidal Wipes) are proven more effective than chlorine against hard-to-kill organisms in real clinical environments. They are shown to reduce the total counts of aerobic and anaerobic organisms10, to be more effective at reducing persistent Gram-negative organisms11 and to reduce the incidence of C. difficile-associated disease by 72%12.
As we uncover the interaction between disinfectants and dry surface biofilms, we make better-informed decisions about our infection prevention policies. Ongoing and emerging research highlights a clear role for the patented Clinell Peracetic Acid Wipes formulation in the battle against high-risk and hard-to-kill organisms13.
To find out more, speak to your local GAMA Healthcare Area Manager or visit www.gamahealthcare.com.
References
1 Suetens et al. Point Prevalence Survey of Healthcare-Associated Infections and Antimicrobial Use in European Acute Care Hospitals. Stockholm: ECDC; 2013.
2 Vickery et al. J Hosp Infect. 2012;80(1):52-55.
3 Hu et al. J Hosp Infect. 2015;91(1):35-44.
4 Otter et al. J Hosp Infect. 2015;89(1):16-27.
5 Ledwoch et al. J Hosp Infect. 2018;100(3):e47-e56.
6 Ledwoch & Maillard JY. Materials (Basel). 2019;12(1):4-13.
7 Ledwoch et al. Lett Appl Microbiol. 2019;68(4):329-336.
8 Humphreys et al. J Infect Prev. 2013;14(4):126-131.
9 Siani et al. Am J Infect Control. 2011;39(3):212-218.
10 Siani et al. Am J Infect Control. 2018;46(10):1180-1187.
11 Saha et al. Am J Infect Control. 2016;44(11):1247-1251.
12 Carter & Barry. Tackling. Nurs Times. 2011;107(36):22-25.
13 Sivaramakrishnan et al. Infect Prev Pract. 2020;2(3):100021.
This article is from issue 18 of Health Europa. Click here to get your free subscription today.
























