
European Federation of Nurses Associations Secretary General Paul De Raeve and President Elisabeth Adams detail the ways in which EFN’s current lobbying efforts parallel the pioneering work and legacy of Florence Nightingale.
Florence Nightingale was born on May 12, 1820 in Florence, Italy, and died on August 13, 1910, in London. Her legacy and influence on society and politics, philosophy, science, education and literature is well documented, demonstrating that on political matters she was an astute behind-the-scenes political activist. She campaigned for legislation on what would become the Public Health Act, which was enacted in 1874.
Nightingale challenged the poor working conditions for nurses and set standards for hospital conditions and patient care which became foundational to the development of modern nursing. She advocated to elevate the nursing profession’s reputation with better educational standards, which in turn encouraged more women to enter the profession than ever before. But she was aware of the limited effect one person could have leading to her mission to reach the people who could put her reforms into practice: MPs, government officials and army officers.
Her views dramatically changed society’s approach to nursing. She understood the valuable contribution that nurses could make to healthcare. She was committed to personalised care, and thus discovered that sensitivity to patient needs was a key to accelerator of recovery. Her voice was strong, and she served as an effective advocate on several important health issues, particularly for trained nursing and preventive health care through proper hygiene. Through her contacts in the government, she influenced public policy and achieved positive healthcare reforms.
Most of her legacy is reflected in the EFN’s ongoing lobbying endeavours at the EU level on behalf of three million EU nurses, lobbying the European Parliament, the European Commission and the European Council.
The ‘mother’ of modern nursing
Among other issues, Nightingale campaigned for legislation that would make connecting with main drainage systems mandatory for all buildings. Moreover, she raised her voice to openly challenge the poor working conditions for nurses and demanded new standards for hospital conditions and patient care which would later become foundational to the development of nursing as we know it today.
Much of her advocacy work aimed at elevating standards in nursing education, which in turn encouraged more women to enter the profession than ever before.
Nightingale worked as a nurse during the Crimean War. On her return to London in 1856 she set about publicising her statistical findings as well as her proposed medical reforms – but she was aware of the limited effect one person could have on practices within the armed forces and the nursing profession. Her mission was to reach the people who could put her reforms into practice: MPs, government officials and army officers, few of whom had statistical or scientific training. One of Nightingale’s most significant innovations was a diagram which showed the causes of soldiers’ deaths over two successive years in the Crimea (Fig. 1).
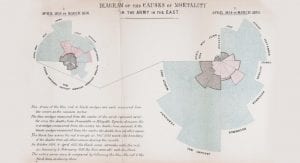
The diagram illustrates two key points: the first is that the reforms Nightingale implemented and campaigned for made a huge positive difference to mortality. The second, more shocking result is that more soldiers died from preventable diseases during the war than from injuries. Nightingale was one of a small group of mathematicians who seized on the power of graphics to describe statistical findings to a non-specialist readership.
Following the example set by Nightingale, the EFN is continuously working at the EU level to improve the nursing profession at all levels possible, and to empower those who are devoting its life towards it. With this goal in mind, the EFN is actively working on a series of EU files which affect the nursing profession, as detailed below.
The European Pillar of Social Rights
The European Union, as an economic project, oversees the Single European Market for the ‘free movement’ of people, goods, services and capital: to include the nurses’ voice in the co-design of new EU legislation is key. In this context, the project of building a social Europe comes high on the political agenda, with civil society taking a proactive approach to lobby strategies which aim to make a difference. The European Commission has adopted that idea and developed it into the European Pillar of Social Rights, a ‘soft law’ designed to act as a policy tool for EU policymakers to foster the involvement and rights of the civil society on the EU’s policy development and outcomes.
The 20 principles enshrined in the European Pillar of Social Rights aim to address crucial topics such as equal opportunities and access to the labour market; fair working conditions; and social protection and inclusion. The key for the EFN, therefore, is ensuring that these principles can be integrated into concrete policies and actions which support the daily practice of three million EU nurses.
Considering the increasing pressure faced by the European healthcare and social systems, it is central to invest in a motivated and skilled nursing workforce delivering frontline care. Addressing the unmet needs of nurses throughout the EU cannot be further postponed, with the situation for nurses deteriorating beyond terrible levels, impacting on their ability to deliver appropriate safe and quality care many nurses see the only choice is to leave the profession. Without appropriate and timely policy measures from within the European Pillar of Social Rights, nurses will become difficult to be recruited to and retained into the job.
Anyone who has ever experienced, either as patient or relative, the need of receiving healthcare knows that without the nurses, these high qualified services could be no longer provided.
Cross-border healthcare
Although health policy, including the organisation, financing and management of healthcare, remains a national responsibility of Member States, the development of health policies at EU level, although the EU as a body has no direct expertise in this field, has been coming at speed since 2000; and at even higher speed since 2010. As the EU institutions reached a political agreement on the Directive on Patients’ Rights in Cross-Border Healthcare in 2014, implemented weakly since 2013, nurses play an important role in understanding better the potential upcoming challenges for patients and making sure the European Commission recognises their input.
The EFN and the nurses’ role in the continuity of care within this Directive, next to designing nursing sensitive criteria, is central in co-designing health policies. The EFN advocated for the key principles and strategies required for the optimal implementation of continuity of care, which relate to continuity of communication and information between primary and secondary care and between health and social care providers, in order to provide a holistic and integrated care for European citizens based on individual needs. Deployment of community care facilities equipped with interoperable telehealth services to support channels of communication is central. The EFN believes that high standards of co-operation, active flows of communication, team working and a multidisciplinary approach within integrated delivery systems are key to put flesh on the bones of the Directive 2011/24/EU on patients’ rights in cross-border healthcare.
The legal framework is highly complicated and unless simplified, it creates a dysfunctional system. Reasons such as high costs and language barriers are often cited as factors in the Directive’s failure to achieve its full potential. This shows that besides informed patients, we also need a better systemic collaboration. The EFN has cross-border healthcare on its political agenda and continues lobbying at the EU level to make it a tangible reality.
Nurses’ education in EU law
The 1957 Treaty of Rome established the principle of free movement, which acted as a catalyst for many subsequent developments in health and education. This, in turn, translated into some professions being regulated at the EU level, in order to ensure automatic recognition across all EU countries. These seven sectoral professions – midwives, nurses responsible for general care, doctors, dental practitioners, pharmacists, veterinary surgeons and architects – have a special regime, while all other regulated professions benefit from the general system.
The Sectoral Directives set out the minimum standards required for the nature, content and length of education and training programmes leading to a qualification which would be automatically recognised by all Member States for seven specific professions. The battle to establish these minimum standards – and the developing co-operation within EFN which enabled nursing to play a significant role in their creation – is a key part of the history of the European nursing movement, and a major landmark for nursing.
Then, in 2005, after three years of active lobbying at National and European levels, a new ‘Directive 36’, simplifying and consolidating the existing rules and procedures, was adopted; thus safeguarding the European Nursing Directive. The new Directive provides better protection of public interest and public health in the free provision of services and the legal certainty for the direct input of the professions within the consultation mechanism is safeguarded. High quality nursing saves lives: a 2016 study1 showed that a slight increase of 10% in the proportion of nurses holding a bachelor’s degree in nursing reduced the risk of patient death by 5%.
The EFN continued lobbying MEPs and Council representatives, as well as tabling amendments to the rapporteurs of the relevant committees in the European Parliament. There may have been stumbling blocks and setbacks along the way, but the persistence and grit shown by the EFN and its members have not gone unnoticed by key politicians. During the EFN roundtable held in the European Parliament in September 2012, discussions showed the willingness of permanent representations, MEPs and the European Commission to collaborate with nursing leaders in shaping the compromises that will ensure the right balance between mobility and high-quality delivery of health care. “Our major concern as policymakers is to ensure that our policy goals when legislating in the Internal Market do not hamper the highest possible levels of quality and safety in healthcare provision to our citizens”, said Phil Prendergast MEP.
The EFN also agreed on and finalised common amendments with five other sectoral professions – midwives (EMA), dentists (CED), doctors (CPME), pharmacists (PGEU) and veterinarians (FVE) – which were tabled to the European Parliament. The continuous dialogue between EFN and the European Commission has been crucial in exchanging views on the 12-year entry requirement, the update of Annex V, partial access, and delegated acts.
The EFN continued monitoring developments very closely. The European Commission Internal Market Directorate General, the Cypriot and Irish EU Presidencies, ‘the trialogue partners’ and the EFN supported Bernadette Vergnaud MEP in getting the Council to introduce eight learning outcomes, with the opportunity, through delegated acts, to reform nursing education in the EU. We can therefore say that the successful point from the challenge of updating nurse education requirements is the inclusion of eight key descriptors as learning outcomes that focus on the content and quality of the nurse education and as such tries to harmonise the different nursing education pathways.
The approved modernised Directive became a positive legislative outcome which strengthens the minimum requirements for the nursing profession and empowers the nurses in the future healthcare systems. The EFN continued leading the design of Annexe V through delegated acts and made sure the profession and regulators started speaking with one voice.
Therefore, in 2016, the EFN held several meetings with the European Commission representatives from DG GROW (DG Internal Market, Industry, Entrepreneurship and SMEs) to discuss the preparation of a delegated act updating the Annex V, involving as many stakeholders as possible in the process. The EFN Secretary General also presented the importance of a delegated act updating Annex V at the European Professional Card (EPC) conference, held on 18 March 2016, embracing future alliances with key stakeholders. As a result, a text that could replace the existing Annex V in the area of nursing has been developed by the EFN and agreed upon by a variety of stakeholders, including the European Regulators Network. The EFN will need to continue the pressure on the European Commission and the National Co-ordinators for the Directive to deliver ASAP a delegated act.
In May 2015 the EFN published its Competency Framework2 which describes the competences required for nurses responsible for general care. The framework has been translated into several languages by EFN members and used by the National Nurses Associations to encourage and guide nursing schools at national level to implement the competences listed under article 31 of the Directive.
The next step for the EFN in this process is the development of a delegated act by making sure that the legislative EU requirements have been correctly and totally implemented at national and regional levels as this is crucial for the quality and safety of the health services delivered by nurses. Therefore, the challenge for the third decade of the 21st century remains again how to strengthen the Directive and the nursing profession, whilst safeguarding it against shortsighted economic austerity measures which aim to reduce cost at the expense of public health.
The Proportionality Directive
The EFN has opted in favour of the controversial Proportionality Directive, adopted in 2018, on the basis that it could arrest the tremendous downgrading of nursing in many Member States. Some national governments kept creating new teaching programmes and legislation for the development of a ‘lower level nurse’. Therefore, the Directive was perceived by EFN as a positive tool to develop new regulation related to advanced roles for nurses.
We need EU legislative tools to help the NNAs developing nursing in the coming years. The Proportionality Directive became an extra safeguard in trying to ensure that countries do not get around the minimum nurse education requirements by creating new nursing professions and assistant roles which are not ‘general care’ nurses. In some countries, the Professional Qualifications Directive is being flouted, with governments trying to bypass the European legislation and create a new model of nursing education, replacing general care nurses with cheaper, lower qualified nurses, with a lower salary; and outsourcing tasks from general care nurses to lower qualified staff.
Transparency and stakeholder engagement are key in the Proportionality Directive, a concept which is more talked about then implemented. We need EU legislative tools to support the NNAs developing nursing throughout the EU and Europe as governments often decide without any consultation. As such, the EFN will continue ensuring that the level of protection of public health will not be undermined by the new provisions and that EU citizens will continue enjoying access to appropriately trained and regulated professionals.
The Sharp Injury Directive
An important example of impact the EFN has on European policymaking is one which strikes close to home for nurses. Sharps injuries, and particularly needlestick injuries, bring the risk of potentially life-threatening infections into the daily working life of millions of health care providers. More than 30 dangerous bloodborne pathogens are transmitted by contaminated needles, including hepatitis B, hepatitis C and HIV. The bore of the needle acts as a reservoir for blood and other body fluids and small amounts of blood can result in potentially life-threatening infection. Additionally, the emotional impact of a sharps injury can be severe and long lasting, even when a serious infection is not transmitted.
Sadly, every year in Europe approximately 1.2 million needlestick injuries are suffered by healthcare staff (European Commission, 2009). A study from one European country reported that needlestick injuries were the most reported type of significant exposure, with 63% of those injuries caused by hollow bore needles. 45% of these occurred amongst nursing professionals and 37% amongst medical professionals. A much lower incidence was identified amongst professions allied to medicine and ancillary staff, with most being sustained from inappropriately discarded needles in rubbish bags. Another European country study reveals that the highest risk area for the likelihood of needle-stick injury is venous blood drawing (>38%), and that only 20–50 % of all needle-stick injuries are reported.
There is a huge body of independent evidence demonstrating that most of these injuries are avoidable if workers are provided with the correct protection. As well as safeguarding the safety of healthcare staff and making this a more attractive profession, prevention measures have been proven to be cost effective (Wittmann et al, 2000). The EFN campaigned to eliminate the risk of needle-stick injury for nurses, focusing upon developing European standards to reduce the use of needles, ensure protection for exposed sharps through the use of medical devices, and ensuring safe work practices including through better education and training.
Conclusion
Considering Florence’s Nightingale huge contribution to nursing, it is worth noting that most of her legacy reflects what the EFN is still fighting for at the EU level. The mission of the EFN is to strengthen the status and practice of the nursing profession for the benefit of the health of the citizens and the interests of nurses in the EU and Europe; proactively providing nurses’ input to the European Commission and the European Parliament is key for setting the agenda of the European Council. This is a proactive process consisting of equipping the civil servants of the EU institutions with the available nursing evidence, both qualitative and quantitative, to enable actions initiated in those fields in which the EFN Members have agreed on taking action.
For the daily lobbying work carried out by the EFN, it is fundamental that all information, knowledge and experience is shared among all involved EU decision makers, EU stakeholders, and the EFN members. When new laws and policies are developed in co-design with end users, policy outcomes benefit from being better and faster adopted. The EFN’s ‘federal-like’ structure, in which the National Nurses’ Associations decide on the strategic priorities and the lines of lobby action, ensures there is congruence between the policies and priorities in the national arena and the actions taken by the EFN in the EU’s policy and political environment. Lobbying is a fact of public life in all countries. It has the potential to promote democratic participation and can provide decision makers with valuable insights and information, as well as facilitate stakeholder access to public policy development and implementation.
The success of the EFN has been marked by its ability to take advantage of the opportunities which the European Union has offered in the last 50 years; and as such has strengthened the profession of nursing in the EU and Europe. Initially those opportunities were mainly restricted to policies directly related to one of the original aims of the Union – that of freedom of movement. The EFN seized upon this opportunity to foresee a legal foundation for the minimum standards for nursing education throughout the EU, with consequences which have gone far beyond what might have been envisaged in the seventies. Within this political context, the EFN was able to create window opportunities for change and demonstrating the tenacity to keep raising the voices of nurses to policymakers until they could make change happen.
Finally, nurses are and will continue to be part of the objective of the EU in promoting peace, its values and the wellbeing of its people. Nurses continue to advocate for the weakest, the most vulnerable in society; and developed political mechanisms leading to successful policy outcomes and ensuring that Europe’s citizens get the health and social services they need.
References
1 Aiken L. et al (2016) Nursing skill mix in European hospitals: cross-sectional study of the association with mortality, patient ratings, and quality of care. qualitysafety.bmj.com/content/early/2016/11/03/bmjqs-2016-005567.full.pdf
2 EFN (2015) EFN Competency Framework for Mutual Recognition of Professional Qualifications Directive 2005/36/EC, amended by Directive 2013/55/EU: http://www.efnweb.be/?page_id=6897
Professor Dr Paul De Raeve, RN, MSc, MStat, PhD
Secretary General
Professor Dr Elisabeth Adams, RN, Cert (ODN), BNS (Hons), Dip (Mgt), Dip (Counselling), Dip (Phy & Chem), H.Dip (Stats), MSc
President
European Federation of Nurses Associations
http://www.efnweb.eu
This article is from issue 13 of Health Europa. Click here to get your free subscription today.
























