MDxHealth has developed the most comprehensive solution for diagnosing prostate cancer, shifting treatment from a generic approach to a more personalised method.
Across Europe and around the globe, innovators and leaders in healthcare are shifting from a one-size-fits-all mentality to a personalised, patient-centric approach, known as precision medicine, focused on improving patient outcomes, eliminating unnecessary invasive procedures and reducing healthcare costs by utilising the latest advanced molecular tests. Precision medicine offers non-invasive, powerful, accurate and often cost-effective tools to empower physicians to learn more about their patients’ specific conditions and needs, helping them make decisions faster with better outcomes. MDxHealth is a multinational molecular diagnostics company that is leading the precision medicine movement in urological oncology with its SelectMDx and ConfirmMDx for Prostate Cancer tests.
The prostate cancer problem
Prostate cancer is the most frequently diagnosed cancer in European men.1 According to the European Association of Urology (EAU), an estimated 417,000 men are diagnosed with prostate cancer and 92,300 men die from the disease each year.2 Prostate cancer is the second leading cause of cancer death in Europe after colorectal cancer.1
If prostate cancer is caught early, it is almost 100% curable. Unfortunately, the disease is often symptomless in its early stages. Once prostate cancer has metastasized survival rates decrease to 30%.3 For those with aggressive cancer, early detection is crucial to survival.
For patients with non-aggressive prostate cancer, however, diagnosis and treatment can often do more harm than good. There has been a paradigm shift in how urologists treat these clinically insignificant cancers. Instead of subjecting patients to chemotherapy, radiation or surgery, urologists will actively monitor these patients. This slow-growing non-aggressive cancer is harmless in most patients. The treatment and side effects are sometimes more harmful than this grade of cancer.
According to the United States Preventative Services Task Force (USPSTF): ‘Individuals with cancer that is overdiagnosed do not benefit from having their cancer detected by screening but they suffer from the harms of evaluations done to establish that cancer exists and the harms of treatment for the cancer. The harms of treating prostate cancer can be both serious and common.’ In fact, even just a diagnosis of prostate cancer without treatment may cause patients to ‘suffer from anxiety and diminished wellbeing because of the cancer diagnosis and they may be burdened by the testing and interventions used to monitor the cancer’.4
Similarly, the EAU-ESTRO-SIOG Guidelines on Prostate Cancer recommend targeted screening for men at higher risk of prostate cancer. The EAU guidelines also note that ‘breaking the link between diagnosis and active treatment is the only way to decrease the risk of overtreatment while maintaining the potential benefit of individual early diagnosis for men requesting it’.5
The most common prostate cancer screening method is a test that measures the blood levels of prostate-specific antigen (PSA), a protein produced by prostate tissue. While a high level of PSA in the bloodstream may be a warning sign for prostate cancer, there are other non-cancerous conditions by which PSA levels may increase, such as enlargement or inflammation of the prostate.6 In fact, only approximately 25% of men with elevated PSA are at risk for prostate cancer.7 Also, it’s possible for cancer to be present even if one’s PSA is not elevated.8
If a patient has an elevated PSA and other potential symptoms, such as a concerning digital rectal exam, the next step in the traditional prostate cancer diagnosis process would be to order a multiparametric magnetic resonance imaging (mpMRI) test. By creating a cross-sectional image of the prostate, mpMRI provides information about the presence of prostate cancer on a scale of 1-5 (PI-RADS V.2 scoring), where 4 and 5 indicate that aggressive cancer is likely present. However, most mpMRI outcomes will be PI-RADS 1-3, meaning that the presence of less aggressive cancer is less certain. Some cancers cannot be detected by mpMRI. Additionally, these tests can be uncomfortable to the patient and the units are associated with costly set-up, staffing and maintenance.9
The PROMIS study, published in The Lancet, found that using mpMRI as a triage test before an initial prostate biopsy can reduce unnecessary procedures by a quarter9 – helpful, but not the most effective tool for this purpose. Biomarker tests, such as SelectMDx, have shown to more effectively rule out patients who do not have aggressive prostate cancer.
While mpMRI is limited in its ability to prevent unnecessary procedures, it can still play an important role in the diagnostic pathway by indicating where the cancerous cells are located within the prostate – useful information when performing a biopsy.
Transrectal ultrasound-guided biopsies are considered the ‘gold standard’ for diagnosing prostate cancer but are invasive for the patient and can be associated with side effects such as infection, bleeding and other complications — some serious enough to require hospitalisation. Up to 30% of patients who undergo a prostate biopsy are at risk for complications, with approximately 4% requiring hospitalisation.10 Additionally, a standard biopsy samples less than 1% of the entire gland, resulting in a 30% risk of missing the cancer.
Additionally, prostate cancer treatment, which can include radiation therapy or prostatectomy, can have serious negative impacts on sexual and urinary function. Men with ‘good prognosis’ cancer, which typically refers to asymptomatic cancer with a low likelihood of progressing to a more aggressive disease, can actually have worse outcomes due to treatment than if they were placed in active surveillance.
“For very mild cancers, a urologist may choose to follow it closely without treatment, which is called active surveillance. In these scenarios, the symptoms of the cancer will actually be less harmful than the side effects of the treatment,” explained urologist Michael K Brawer, MD, chief medical officer at MDxHealth. “Doctors will closely follow and screen men in active surveillance so that they can begin treatment if and when the cancer progresses.”
For men who have clinically insignificant prostate cancer, active surveillance results in higher quality of life and less negative impact on sexual and urinary function.11 Additionally, studies have found that active surveillance does not have significant emotional impacts on men.12,13
However, a physician’s confident recommendation of active surveillance depends on the amount and quality of data accessible. Molecular diagnostics offer valuable information that empower physicians to make diagnostic and treatment decisions with a higher level of confidence.
The precision medicine solution
Many significant improvements have advanced the science and medicine of prostate cancer diagnosis. Innovations in precision medicine have helped to improve patient risk stratification, more accurately detect aggressive prostate cancer, and reduce unnecessary biopsies.
Molecular diagnostic tests improve the PSA test’s ability to identify patients at risk for aggressive prostate cancer, providing physicians with a more accurate picture of the situation and enabling them to take into account all clinical and laboratory information when working with an individual patient.
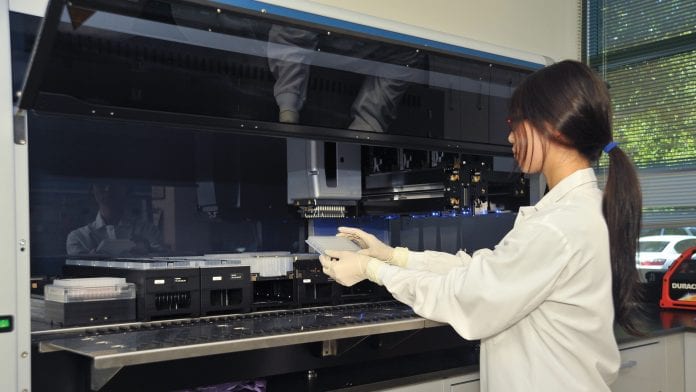
Using a patient’s genomic information and clinical risk factors, MDxHealth has developed two tests that provide a patient’s personalised risk for harbouring a life-threatening disease – SelectMDx and ConfirmMDx. This comprehensive approach addresses the unmet clinical needs in the initial and repeat biopsy setting.
SelectMDx
SelectMDx is a non-invasive urine test used to assess a man’s risk for aggressive prostate cancer and help identify which patients may truly benefit from a biopsy. SelectMDx can be used in men with an elevated PSA level prior to performing an mpMRI, to determine whether a biopsy would be beneficial. The test measures the amount of two genes that are associated with aggressive prostate cancer. This is then combined with clinical information to calculate the likelihood of harbouring aggressive prostate cancer:
- Men identified by the test as having a high probability of aggressive cancer can, upon biopsy, be diagnosed and treated sooner, while men identified at very low risk may avoid biopsy
- The test’s negative predictive value is 98%, meaning if the test identifies a very low risk, the physician and patient can be 98% sure the patient does not have Grade Group ≥2 (Gleason score ≥7) or no prostate cancer and avoid a biopsy1
- SelectMDx can rule out patients who do not have clinically significant cancer, preventing unnecessary mpMRI and biopsy procedures. For patients whose SelectMDx results indicate the presence of cancer, an mpMRI can then be ordered to help identify where the cancer is located in the prostate before performing a biopsy, resulting in faster, more accurate diagnoses
- A study published in Prostate Cancer and Prostatic Diseases found that utilisation of SelectMDx in the initial diagnoses of prostate cancer resulted in reduced costs and gains in quality-adjusted life years in France, Germany, Italy and Spain.14
Just recently, a study published in Urology Practice demonstrated that SelectMDx had a significant impact on initial prostate biopsy decision making. The study demonstrated that urologists were five times more likely to biopsy a patient with a SelectMDx positive result than a patient with SelectMDx negative result – showing that urologists have confidence in the test’s results.
ConfirmMDx
Urologists also deal regularly with the challenges of prostate biopsy sampling errors and false-negative biopsies. To address this dilemma, MDxHealth developed ConfirmMDx, a tissue test that can be performed after a patient has undergone a biopsy with a negative result.
While the PSA test is the gold standard for prostate cancer screening, only a biopsy of the prostate gland, most often using transrectal ultrasound guidance, can establish the diagnosis of prostate cancer. Although these biopsies are considered the standard of care, studies have shown they miss detecting up to one-third of men who have prostate cancer.
The 12-core standard biopsy schema samples less than 1% of the entire prostate gland and results in limited histopathological analysis. Sampling error is an inherent and well-documented issue, with false-negative rates as high as 25-35%.15,16 Additionally, 43% of patients with negative histopathology on initial biopsy will undergo a repeat biopsy, many also continuing on third and fourth biopsies – resulting in significant costs and increased risk of infection and hospitalisation.16,17
Rather than perform repeat biopsies on patients without prostate cancer, urologists with persisting concern about missed cancer in a patient can order the non-invasive ConfirmMDx test. The test, used on the tissue that was being stored from a patient’s last biopsy, can rule out a false-negative biopsy result with a 96% negative predictive value. Since an additional biopsy isn’t required for this test, physicians can save resources and spare patients from undergoing the painful, invasive procedure again if cancer is ruled out.
ConfirmMDx uses the epigenetic field effect, meaning that tissue adjacent to the cancer foci can contain DNA methylation changes, which are invisible by histopathologic review, but detectable by methylation-specific PCR (MSP). Detection of a methylation signal suggests a nearby cancer focus, even though the needle biopsy did not identify the prostate cancer.
The ConfirmMDx test, if positive for DNA methylation, will help identify those patients at risk for aggressive prostate cancer that would benefit from a repeat biopsy.18
The promise of molecular diagnostics
Physicians are ethically burdened to deliver the best personalised care but are increasingly asked to stretch resources to deliver results. The balancing act between overutilisation and underutilisation to deliver precision medicine – the right care at the right time to the right patient – has never been more acute. MDxHealth’s technology platform is helping urologists meet the challenge in prostate cancer diagnosis and treatment with its SelectMDx and ConfirmMDx tests. These tools provide physicians with essential information that will continue to increase confidence in clinical decision making, reduce unnecessary procedures, and, most importantly, improve patient outcomes.
MDxHealth has a global prostate cancer portfolio vision to improve the standard of care. In addition to focusing on guideline inclusions, this outlook includes validating SelectMDx for active surveillance as well as in the primary care setting. Furthermore, MDxHealth is developing two LDT tests – InformMDx and MonitorMDx for Prostate Cancer.
References
- Cancer statistics – specific cancers. (2018, July). Retrieved from https://ec.europa.eu/eurostat/statistics-explained/index.php/Cancer_statistics_-_specific_cancers
- Mottet N et al. Members of the EAU – ESTRO – ESUR –SIOG Prostate cancer Guidelines Panel. EAU – ESTRO – ESUR – SIOG Guidelines on Prostate Cancer. Retrieved from: https://uroweb.org/guideline/prostate-cancer/ Access date 3 December 2018
- National Cancer Institute. Cancer Stat Facts: Prostate Cancer. Retrieved from https://seer.cancer.gov/statfacts/html/prost.html
- Contextual Review: Overdiagnosis in Prostate Cancer Screening Decision Models: Prostate Cancer: Screening. U.S. Preventive Services Task Force. October 2018 https://www.uspreventiveservicestaskforce.org/Page/Document/contextual-reviewoverdiagnosis-in-prostate-cancer-screening/prostate-cancer-screening1
- Mottet N et al. EAU-ESTRO-SIOG Guidelines on Prostate Cancer. Part 1: Screening, Diagnosis, and Local Treatment with Curative Intent. European Urology, Volume 71, Issue 4, 618-629 https://www.europeanurology.com/article/S0302-2838(16)30470-5/fulltext
- National Cancer Institute. Prostate-Specific Antigen (PSA) Test. Retrieved from http://www.cancer.gov/types/prostate/psa-fact-sheet
- MDxHealth Annual Report 2017. Retrieved from https://mdxhealth.com/sites/default/files/financialreports/en/2017_AR_EN_Final_POSTPublication.pdf
- Prostate cancer screening: Should you get a PSA test? (1 November 2018). Retrieved from https://www.mayoclinic.org/diseases-conditions/prostate-cancer/in-depth/prosta
te-cancer/art-20048087 - Ahmed HU et al. Diagnostic accuracy of multi-parametric MRI and TRUS biopsy in prostate cancer (PROMIS): a paired validating confirmatory study. The Lancet, Volume 389, Issue 10071, 815-822
- Chamberland RR (2016) Cutting to the core of the issue: emerging strategies to reduce prostate biopsy-related infections. Journal of Clinical Microbiology. 54:2431-2435
- Donovan Jenny L et al. (2016) Patient-Reported Outcomes after Monitoring, Surgery, or Radiotherapy for Prostate Cancer. N Engl J Med 375:15, 1425-1437. Retrieved from https://www.nejm.org/doi/10.1056/NEJMoa1606221
- SUO 2017: Prostate Cancer Anxiety in Men Undergoing Active Surveillance. (n.d.). Retrieved 3 December 2018, from https://www.urotoday.com/conference-highlights/
suo-2017/suo-2017-prostate-cancer/100219-suo-2017-prostate-cancer-anxiety-in-men-undergoing-active-surveillance.html - Bellardita Lara et al. How Does Active Surveillance for Prostate Cancer Affect Quality of Life? A Systematic Review, European Urology, Volume 67, Issue 4, 637-645. Retrieved from https://www.europeanurology.com/article/S0302-2838(14)01101-4/fulltext
- Govers TM et al. (2018) Cost-effectiveness of SelectMDx for prostate cancer in four European countries: a comparative modeling study. Prostate Cancer and Prostatic Diseases, 1
- Crawford D, et al. (2017) Clinical Considerations after a Negative Prostate Biopsy. J Pros Canc 2:1
- Trock BJ, et al. (2012) Evaluation of GSTP1 and APC methylation as indicators for repeat biopsy in a high-risk cohort of men with negative initial prostate biopsies. BJU Int 110: 56-62
- Pinsky PF, Crawford ED, Kramer BS, et al. Repeat prostate biopsy in the prostate, lung, colorectal and ovarian cancer screening trial. BJU Int. 2007;4:775-779
- MDxHealth. ConfirmMDx for Prostate Cancer. Retrieved 3 December 2018, from https://mdxhealth.com/confirmmdx-prostate-cancer-for-patients
Jean-Marc Roelandt
Chief Financial Officer
MDxHealth SA
+32 4 257 70 21
jean-marc.roelandt@mdxhealth.com
https://mdxhealth.com/
Please note, this article will appear in issue 8 of Health Europa Quarterly, which is available to read now.






















