Rebecca Swann and Jason Kasraie of the Association of Reproductive and Clinical Scientists highlight developments in IVF and reproductive science.
The Association of Reproductive and Clinical Scientists (ARCS) is the professional body supporting the needs and research and development interests of those involved in reproductive sciences in the UK. ARCS, founded in 2020 from the merger of three individual professional societies (the Association of Clinical Embryologists, the Association of Biomedical Andrologists and the British Andrology Society), is dedicated to advancing reproductive science through training and education, providing information, support and a global community for its over 700 members. ARCS is led by an experienced and knowledgeable Executive Committee comprised of individuals working within all aspects of reproductive science in both the public and private sectors, ensuring a representative and respected voice of the members. ARCS is recognised by international governing bodies, educational institutions and professional societies as a leading authority in the field.
Technology in reproductive science
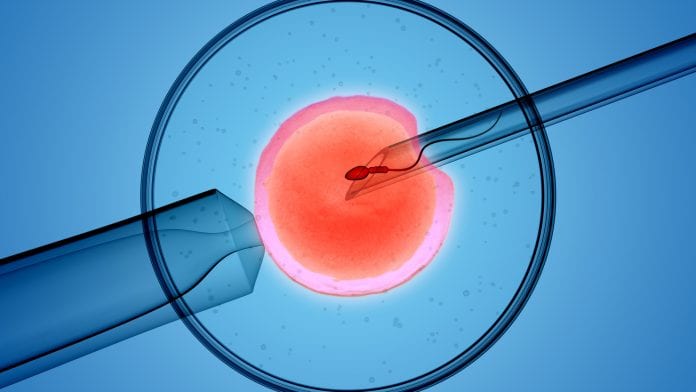
Reproductive science, both clinically and academically, is dependent upon accuracy and consistency. Traditionally the use of digital technology in reproductive science has involved investigation into determining and maintaining basic laboratory conditions; whereas more recently, digital technology has been at the forefront of both precision research and evidence-based clinical advances, in order to ensure optimal embryo development and selection and improved outcomes for our patients. It could be argued that the In Vitro Fertilisation (IVF) procedure and fundamentals of embryo culture are well established, but almost static; and novel technologies and tests are needed all the time to create the incremental gains which result in improved clinical outcomes for patients. It is without a doubt that the integration of digital technology into reproductive science has enhanced our understanding of embryo development, enabled meticulous attention to detail and encouraged clinic-specific improvements for the benefit of our patients.
The IVF laboratory aims to provide, as closely as possible, an optimal in vitro environment for gametes and embryos to thrive. The incubator is the main constituent part of any IVF laboratory and, with the use of digital technology, is able to maintain internal temperature and gas concentrations very precisely and accurately. This internal environment, thanks to the use of digital technology, is under continual monitoring 24/7 and any deviation from the ideal triggers both an audible and external alarm. It is this consistent, optimal environment, which aims to ensure embryos are able to develop to their full potential in vitro.
Process and protocol
The workings of an IVF clinic reflect a protocol-driven approach to ensure adherence to regulations and safety for patients’ gametes and embryos. An integral part of ensuring safety for gametes and embryos at every step of the treatment pathway is through the witnessing procedure. Witnessing is an essential step prior to any procedure within the IVF clinic, either through confirming the identity of a patient prior to consultation or confirming the identity of patient’s gametes prior to them being mixed together. Witnessing within the IVF laboratory most often involves two colleagues confirming a series of unique patient identifiers prior to each procedure. In response to unfortunate events involving ‘mix-up’ of patient material the UK’s regulatory body, the Human Fertilisation and Embryology Authority (HFEA), directed strict guidelines with regards to the witnessing procedure. These changes catalysed developments in digital technology to apply the use of RFID tags to enable electronic witnessing in the IVF laboratory. These systems were not designed to supersede manual witnessing, but instead to support the witnessing procedure, enhancing workflow within the laboratory, enabling traceability of witnessing events and ultimately improving safety both for the patient’s material and for staff.
Once embryos are created in vitro they are cultured within an incubator for up to seven days, demonstrating development from the cellular stage to the blastocyst stage. Embryo quality is evaluated throughout development, with a final decision most commonly made by the embryologist at the blastocyst stage whether to transfer or freeze, one or more embryos, based on a patient’s treatment plan and clinical history. With the use of digital technology, embryo evaluation and selection has significantly changed over the past few years. A number of incubators are now available which have an integrated camera able to capture an image of an embryo every few minutes, creating a timelapse video of development. The timelapse video software has significantly advanced our understanding of embryo development and has led to the application of morphokinetic and morphodynamic models of embryo development based on live birth outcomes. These models are capable of highlighting potential ‘indicators’ of both optimal and suboptimal embryo development, which can influence embryo selection for transfer and freezing. This software continues to develop with research currently being undertaken into the application of Artificial Intelligence, algorithms and computer learning to continually develop and change models to improve embryo selection and associated success rates.
Continuing professional development
At ARCS we support research and development and training for our members. It is part of our professional responsibility as registered clinical scientists with the Health and Care Professions Council (HCPC) to maintain continuing professional development (CPD). In recognition of this, ARCS have their own CPD scheme with reviews and certification awarded for our members every five years. The CPD scheme acknowledges differing areas of CPD, ensuring a balanced approach to all aspects of professional responsibilities. ARCS offers a number of training events, promotes other training events, Journal-Based Learning, online modules and opportunities to write for publications and present during annual conferences. The ARCS CPD scheme supports members in their professional development, to expand their knowledge and keep abreast of advancements in the sector to ensure clinics are able to offer the best care for patients, their gametes and their embryos.
COVID-19
The COVID-19 pandemic, as for all sectors, has imposed significant changes for the world of IVF. The ARCS Executive have been actively reviewing both national and international guidance from both the global reproductive science community and the UK government to provide appropriate support and guidance for our clinics, colleagues and patients within the UK. In accordance with government and health service guidance, on 18 March 2020 ARCS released a joint statement with The British Fertility Society (BFS) to recommend the cessation of all IVF treatment, except for extremely urgent cases (for example, preservation of fertility for cancer patients). Patients who were already in treatment at the time of the closedown were able to complete their treatment cycle. However, patients were recommended to defer embryo transfer and instead freeze all of their available embryos. Following on from the joint statement, the recommendation was considered and enforced by the HFEA. The ARCS Executive Committee was integral to the development of the guidance and unanimously supportive of the difficult decision to recommend cessation of treatment.
This decision was not taken lightly, but was considered essential in order to eliminate the risk to patients who would not be able to adhere to social distancing during treatment as well as eliminate the potential strain on the National Health Service (NHS) through complications, such as Ovarian Hyperstimulation Syndrome (OHSS), that can arise as result of IVF. Since stopping IVF treatment, staff within NHS IVF clinics have been undergoing retraining in preparation to be redeployed as support staff during the pandemic; while staff in private centres have been contacted through ARCS to encourage them to consider volunteering for the same. Although treatment cycles may have stopped, clinics continue to engage with their patients utilising digital platforms to provide counselling and support, as many patients are anxious of their potential decline in fertility as time passes in lockdown. Clinics continue to work to ensure they adhere to regulatory conditions set by the HFEA, monitoring gamete and embryo storage tanks, conducting ongoing audits and fulfilling administration duties.
Preservation of genetic material
Cryopreservation of gametes (sperm and eggs) and embryos is offered for patients by a majority of IVF clinics within the UK. Regulations set out by the HFEA specify that patients choosing to cryopreserve need to consent to the duration of storage, and that material cannot be stored beyond this time. Patients choose to store their gametes and/or embryos for a number of different reasons. Some patients choose to store for fertility preservation as they are to undergo a procedure which would prevent them from being fertile in the future, such as chemotherapy; these patients are able to consent to store gametes and embryos for up to 55 years. Patients who choose to store for social reasons, for example by freezing eggs or embryos for siblings, are able to consent to store their material for up to 10 years. This 10-year limit for storage has recently been brought into question.
Women are encouraged to bank their eggs at a young age due to the fact that egg quality declines with age. However, those individuals electing to freeze their eggs at a young age are now approaching the end of their storage period. For example, a woman in her 20s choosing to store her eggs has to utilise them by her 30s, a time at which she may not yet be ready for treatment and instead is faced with the possibility that her eggs will need to be discarded. Considerations are being made by the HFEA with a view to change the law to reflect these social changes and new opportunities. However, this will take time. A recent consultation by the HFEA to patients and professionals has provided an opportunity to voice views and suggestions with regards to potential changes to the law. Changes, if any, will be challenging logistically as they must reflect both patient and clinic concerns and during this time some patients may even reach their storage limit with few options available for them. For clinics, changes in the law may provide an opportunity for their patients to extend storage, so contingencies will need to be in place to contact these patients and obtain appropriate consent, ensure sufficient capacity to store and manage all cryopreserved material and to maintain contact with patients over a longer period of time.
Future developments
The field of IVF could be considered a relatively young science, celebrating the 40th birthday of the first ‘test tube’ baby Louise Brown in just July 2018. Any changes within reproductive science stem from extensive research and controlled clinical trials. Some more notable recent developments include the application of embryo screening techniques in an attempt to eliminate certain heritable diseases (Preimplantation Genetic Diagnosis, or PGD) and development of mitochondrial donation and transfer techniques to prevent transmission of mitochondrial disease. Researchers have also explored far-reaching and novel applications in sectors beyond human IVF such as the development of ‘sperm robots’ for cancer drug delivery and preservation of endangered species such as the northern white rhino and certain amphibian species.
Rebecca Swann BSc (Hons), MSc
Jason Kasraie BSc (Hons), MSc, FIBMS, FAHCS, FRCPath
Association of Reproductive and Clinical Scientists
This article is from issue 13 of Health Europa. Click here to get your free subscription today.
























