PrevahexCHX™ antimicrobial dressings use a unique antimicrobial impregnated technology in thin film polymers that is revolutionising the final step in infection prevention.
Preventing healthcare-associated infections (HAIs) is of the utmost importance for healthcare facilities all over the world, and doing so can be quite challenging. An estimated 722,000 HAIs occur annually1 within the US healthcare system’s acute care population. This means that approximately one in 25 hospitalised patients will acquire an infection.
As a result, 75,000 deaths occur annually as a result of HAIs2. Among these HAIs, two are of vital importance: central line-associated bloodstream infections (CLABSIs) and surgical site infections (SSIs). CLABSIs cost facilities approximately $45,000 per infection, and their mortality rate is a staggering 33%. In the US, there are 250,000 catheter-related bloodstream infections (CRBSIs) each year.
Patients with both central venous catheters and peripheral catheters are at risk for infection. Each year, 25,000 deaths are caused by CLABSIs. SSIs cost up to $60,000 per infection, averaging between $12,000 and $35,000 per infection3. SSIs occur in 2% to 5% of all inpatient surgeries; and patients who undergo surgery are at risk for infection for at least 30 days post-surgery.
Both HAIs are caused by bacterial flora on the patient’s own skin. In fact, 60% of catheter-related blood stream infections are caused by microorganisms from a patient’s skin4. As such, facilities try to prevent these infections by using highly efficacious skin antiseptics, with active ingredients such as chlorhexidine gluconate and isopropyl alcohol.
These antiseptics are known for penetrating the first two layers of the epidermis where 80% of resident and transient bacteria reside; however, newer research has shown that post skin antisepsis, regrowth of bacteria occurs within eight hours. Moreover, if just one colony forming unit (CFU) of bacteria remains, the site can become 100% recolonised within 30 minutes5,6. This reoccurrence is happening despite skin preparation because bacteria continue to migrate to the surface. This highlights the need for additional, continuous antimicrobial protection at preoperative, postoperative and catheter sites.
Innovating thin film technology
Founded in 2012, entrotech life sciences, inc (ELS) is a privately held materials science company that specialises in thin film technologies. Jim McGuire, CEO of entrotech life sciences, inc, was focused on developing lifesaving non-antimicrobial polymer film technologies specifically designed for tactical combat casualty care products for the US Military’s Special Forces. When he heard about HAIs and the challenges they pose to healthcare professionals, he was determined to develop an innovative new infection control technology to continue to save lives. With that mandate, he developed the PrevahexCHX™ antimicrobial transparent thin film dressing.
“Evidence shows that catheter-related bloodstream infections and surgical site infections continue to cause unnecessary illness, healthcare costs, and deaths in hospitals across the US,” said Jim McGuire, CEO of entrotech life sciences. “That’s why the entrotech life sciences team developed a groundbreaking product that unlocks the true potential of pure chlorhexidine alongside the innovative technology of a transparent, PCA-free film to advance our mission to prevent infection and create better patient outcomes.”
PrevahexCHX is the first and only pure chlorhexidine (CHX) dressing cleared by the FDA with complete antimicrobial protection throughout the transparent areas of the dressing. PrevahexCHX antimicrobial dressings incorporate groundbreaking technology utilising pure chlorhexidine (CHX), providing rapid, broad spectrum dressing protection at wound and catheter sites.
This technology is currently available in four different dressing types that are appropriate for both vascular and surgical applications.
The chlorhexidine advantage: pure chlorhexidine (CHX)
Chlorhexidine is a highly effective, broad spectrum, persistent antimicrobial that has been effectively used in the healthcare market for more than 60 years7. Pure chlorhexidine (CHX) is the chemical entity that provides the antimicrobial action of the chlorhexidine-based antimicrobials commonly used in healthcare which include chlorhexidine gluconate (CHG), chlorhexidine diacetate (CHA), and a few other less common salts. While pure chlorhexidine (CHX) is a powerful and effective antimicrobial, its chemical structure makes it very challenging to industrially incorporate into solutions and blend into polymers, gels, etc.
As a result, most companies have elected to mix their CHX with either gluconic acid or acetic acid to make the CHG and CHA compounds, respectively, which are much easier and simpler to industrially blend into solutions and materials. There is no evidence that gluconic acid and acetic acid provide any benefit in efficacy, they are both known to cause skin irritation at higher concentrations, and there is evidence suggesting that the presence of these acid additives may suppress the accessibility of chlorhexidine from within dressings8-12.
In contrast, ELS has developed a patented, proprietary process for industrially incorporating pure CHX into our dressings which makes PrevahexCHX extremely effective at killing microorganisms; it is also the only available chlorhexidine dressing 100% free of acids, salts, and binders. In addition, most existing antimicrobial dressings require moisture, alcohol, water or sweat to activate the antimicrobial. These are unfavourable conditions for optimal dressings. Our technology does not require these activators; our dressing works on contact with the patient’s skin. Lastly, because this antimicrobial is integrated directly into the transparent areas of the dressing, the patient receives antimicrobial protection while the clinician is always fully able to see and assess the site. This is a unique feature of our dressing as compared to other antimicrobial dressings on the market today.

A better chlorhexidine, a better dressing
To maximise using an antimicrobial dressing at wound and catheter sites, it is important that this technology activates on contact and provides continuous and consistent release of the antimicrobial to provide full site protection.
PrevahexCHX has demonstrated this ability through in vitro log10 reduction antimicrobial efficacy testing. As part of that test, we made sure to test a broad spectrum of microorganisms, including gram-positive bacteria, gram-negative bacteria, and yeasts as well as several drug-resistant microorganisms. The pathogenic microorganisms included in this study were specifically selected due to their clinical relevance and prevalence as the cause of challenging hospital-associated infections in healthcare. Antimicrobial efficacy was evaluated at one, three and seven-day timepoints and PrevahexCHX consistently achieved greater than 5.0 log10 reduction at all time points demonstrating ≥10x the antimicrobial performance requirements established by the FDA.13 In addition, PrevahexCHX demonstrated rapid onset of action starting at Day 1 and continuing through Day 7, thus dramatically outperforming other competitive antimicrobial dressings which can take several days to demonstrate significant efficacy.
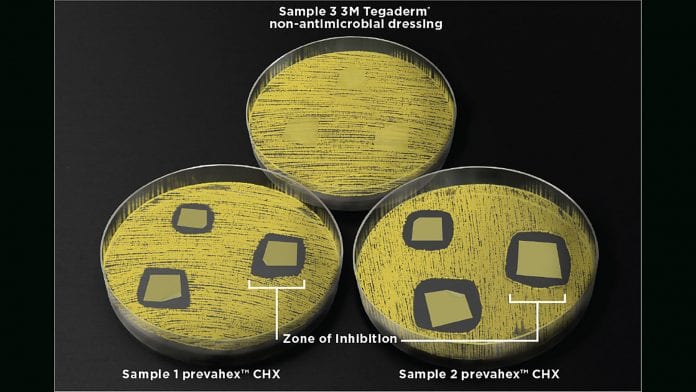
PrevahexCHX is the only antimicrobial dressing on the market that can offer complete CHX protection throughout the transparent areas of the dressing. This level of protection creates the best opportunity to reduce the risk of catheter-related bloodstream and surgical site infections. Zone of Inhibition (ZOI) testing demonstrated rapid bacteria elimination of multiple drug-resistant bacterial species both directly underneath and several millimetres beyond the perimeter of the dressing.
The patented process for manufacturing PrevahexCHX is cleaner, safer and provides us a pathway to incorporate CHX into our adhesive polymerisation process, while eliminating the unwanted side reaction creating p-chloroaniline (PCA). PCA is an acutely toxic skin sensitiser and possible carcinogen found in other chlorhexidine dressings. This is because traditional adhesive technologies, solvent or water based, typically require heat to dry the carrier medium and those elevated drying temperatures result in the formation of PCAs. Most of the other antimicrobial dressings on the market contain PCAs along with other skin irritating additives.
PrevahexCHX products have been tested at the most fundamental levels to assure peak physical performance. PrevahexCHX has passed all functional testing and met all product specification requirements, in addition to demonstrating at least equivalent performance to the leading dressing manufacturer. These tests include water vapour transmission rate, tensile elongation recovery, peel adhesion and more.
Proven results
Since launching PrevahexCHX in 2018, we have been able to get this product into the hands of clinicians to help prevent infections and create better patient outcomes. One example is at a large Level 1 trauma centre in the Northeast United States: one clinician set out to increase dwell times and decrease complications for peripheral IVs (PIVs) through using a vascular access specialist team and technology bundle called the PIV5Rights (PIV5R)14. PrevahexCHX was chosen as the dressing to use in this new technology bundle. It was chosen specifically as a critical component to protect the site by helping to prevent avoidable complications like CRBSIs, phlebitis, and infiltrations and to stabilise the catheter to prevent dislodgement. Through this approach, the clinician was able to achieve an 89% success rate of the catheter staying in until the end of treatment: a substantial increase on the 15% achieved in standard practice. The PrevahexCHX dressing lasted 96% of the time for the full duration of therapy, whereas the standard dressing only lasted 55% of the time. The complication rate for the overall study was only 11% in the PIV5R group and 40% in the standard practice group. Out of the 11% of complications in the PIV5R group, the PrevahexCHX dressing was never cited as a contributing site symptomatic issue. In addition, there were no instances of site irritation, allergic reaction, or adverse events reported. The PrevahexCHX dressing was significantly more likely to last to therapy completion and contributed to lower overall phlebitis and infiltration rates, likely due to its prolonged suppression of bacterial growth.
In addition to catheter sites, our technology has also been used as a post-operative dressing. A vascular surgeon in the Midwest has been using our dressing on patients who have undergone carotid endarterectomy, lower extremity bypass (all various forms) and many arteriovenous (AV) access procedures, both for new access and revision of established AV access. This usage highlights that this technology is extremely versatile. Based off the various clinical uses and customer experiences, we are confident that a technology like PrevahexCHX will be a game changer for both vascular and surgical markets.
References
- CDC, HAI Data & Statistics, electronically accessed 7/11/2016 from cdc.gov/HAI/surveillance/index.html; Journal of the American Medical Association. Prevalence of Antimicrobial Use in US Acute Care Hospitals, May-September 2011, electronically accessed 7/11/2016 from http://jama.jamanetwork.com/article.aspx?articleid=1911328
- Healthline, CDC: Half of US Hospital Patients Taking Antibiotics; 25 Percent on Two or More, electronically accessed 7/11/2016 from http://www.healthline.com/health-news/half-of-hospital-patients-take-antibiotics-100714
- Rupam Gahlot, Chaitanya Nigam, Vikas Kumar, Ghanshyam Yadav, and Sampa Anupurba, Catheter Related Bloodstream Infections, Int J Crit illn Inj Sci. 2014 Apr-Jun; 4(2): 162-167
- Maki, D.G. Weise, C.E. Sarafin, H.W. A semiquantitative culture method for identifying intravenous-catheter-related infection. New England Journal of Medicine. 1977; 296(23): pp. 1305-1309. Maki, D.G. Alvarado, C.J. Ringer, M. Prospective randomised trial of povidone-iodine, alcohol, and chlorhexidine for prevention of infection associated with central venous and arterial catheters. The Lancet. 1991; 338(8763): pp. 339-343
- Karpanen, T. Worthington, T. Conway, B. Hilton, C. Elliot, T. and Lambert, P. Penetration of Chlorhexidine into Human Skin. Antimicrobial Agents and Chemotherapy. October 2008; pp. 3633-3636
- Maki, D.G., Cobb, L., Garman, J.K., Shapiro, J.M., Ringer, M., Helgerson, R.B. An attachable silver-impregnated cuff for prevention of infection with central venous catheters: a prospective randomised multicentre trial. Am J Med 1988; (85): pp. 307-314.
- Shepard, R.C. Kinmonth, J.B. Skin Preparation and Toweling in Prevention of Wound Infection. British Medical Journal. 1962; 2(5298): pp. 151-153
- Ascenzi, J.M. Handbook of disinfectants and antiseptics. 1996
- McDonnell, G. Russell, A.D. Antiseptics and Disinfectants: Activity, Action, and Resistance. Clinical Microbiology Reviews. 1999; c12(1): pp.
- Senior, N. Some observations of the formulation and properties of chlorhexidine. Journal of the Society of Cosmetic Chemists. 1973; 24(4): pp. 259-278
- Block, S.S. Disinfection, sterilisation, and preservation: Chlorhexidine. 5th ed. 2001; xxii: pp. 1481
- Russell AD, Day MJ. Antibacterial activity of chlorhexidine. Journal of Hospital Infection. 1993; 25(4): pp. 229-38
- Holinga, G., McGuire J. In vitro antimicrobial effects of chlorhexidine diacetate versus chlorhexidine free base dressings. Journal of Wound Care. 2020; Vol. 29 https://doi.org/10.12968/jowc.2020.29.Sup5a.S22
- Steere L, Ficara C, Davis M, Moureau N. Reaching one peripheral intravenous catheter (PIVC) per patient with Lean multimodal strategy: the PIV5Rights™ Bundle. JAVA. 2019;24(3):31-43.

Jim McGuire
CEO
entrotech life sciences, inc.
+1 (415) 513-4494
info@prevahexchx.com
www.prevahexchx.com
This article is from issue 14 of Health Europa. Click here to get your free subscription today.
























