
Abingdon Health explores why the use of lateral flow rapid tests during the COVID-19 pandemic may benefit future testing programmes.
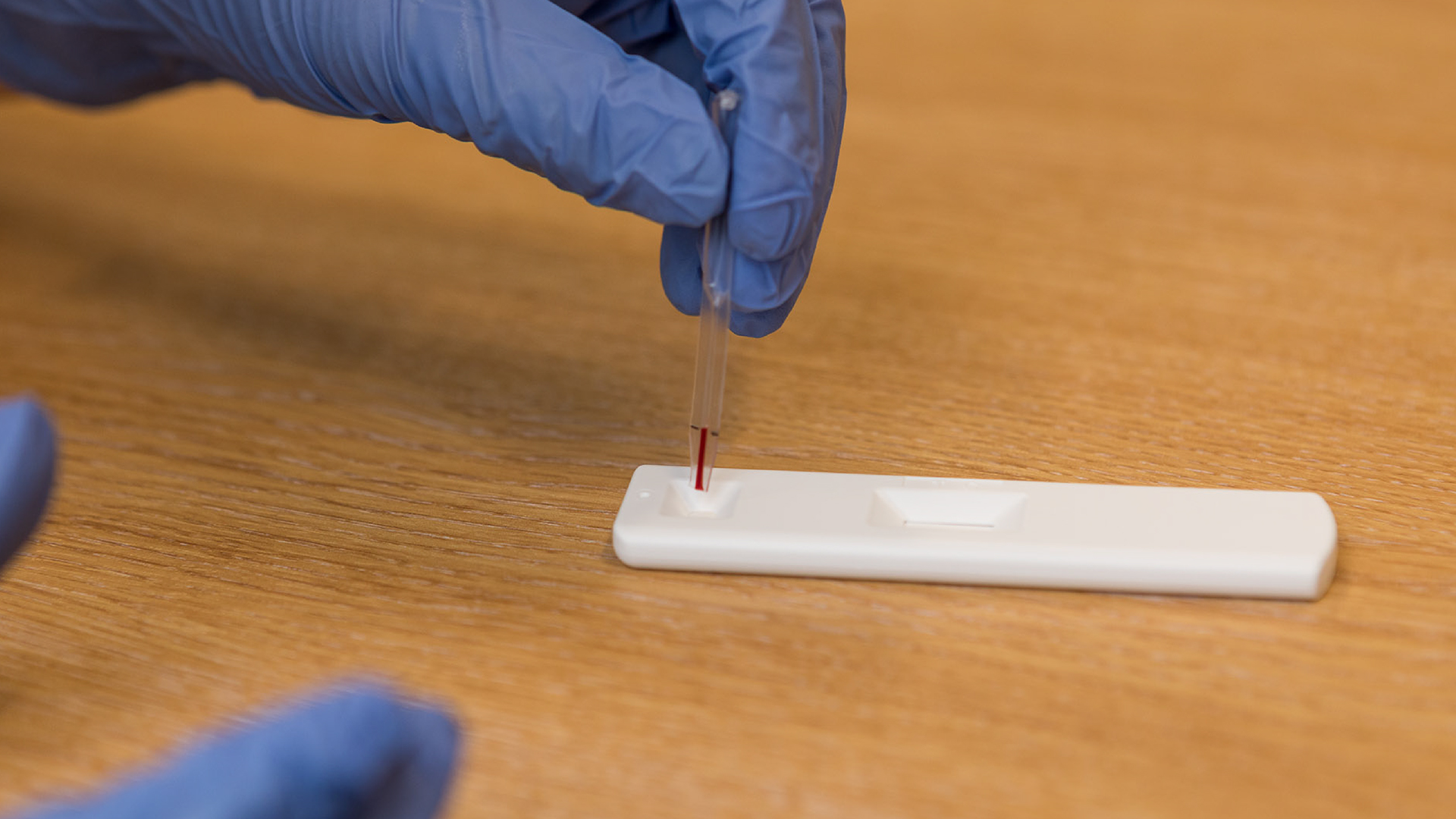
The terms ‘lateral flow’ and ‘rapid test’ have been thrust into the general public’s vocabulary during the SARS-CoV-2 (COVID-19) pandemic, but the technology is not new. For years these easy-to-use devices have been used widely with success: the pregnancy test being the most famous example.
Predictions prior to the pandemic estimated the lateral flow rapid test market would reach approximately $6bn by 2022. One notable example of growth was documented in 2017 by the World Health Organization (WHO), which reported 276 million rapid diagnostic tests (RDTs) for malaria had been supplied globally; with 66% going to sub-Saharan Africa. The report estimated that 75% of all malaria testing in sub-Saharan Africa in 2017 was conducted using RDTs, up from 40% in 2010.
The 2020 COVID-19 crisis accelerated the growth of lateral flow testing, with the market now projected to reach $10.2bn by 2025. This market was growing before the influence of the pandemic; and the latest market growth drivers – the increasing prevalence of infectious disease, ageing populations and the demand for point-of-care testing – were relevant pre-COVID-19 and will remain relevant well into the future.
Abingdon Health, a specialist in rapid test development and manufacture, sees the increased awareness of lateral flow’s patient-centric capabilities as a major factor as to why the technology will be used more widely.
The response to COVID-19
The spread of the ‘new’ coronavirus was fast, and COVID-19 caught many countries off guard. Governments, policymakers, and stakeholders rallied to try and introduce testing strategies that could deliver fast result turnaround times.
Some countries were able to respond more quickly than others. A prime example was South Korea, where between January and March 2020 the state developed and authorised the use of a real-time reverse transcription polymerase chain reaction (rRT-PCR) diagnostic method. By April, 534,552 people in South Korea had been tested for coronavirus.
Throughout the world, organisations mobilised their operations and developed tests in short timeframes; manufacturing capacities were scaled up to meet demand; testing trials and programmes were initiated to quickly assess the state of the COVID-19 situation and formulate response strategies; and vaccine development programmes were initiated across the globe.
During a November 2020 trial in Liverpool, UK, nearly 100,000 lateral flow antigen tests were carried out in a two-week period. Although very important in times of crisis, it was not the volume of tests performed that was of interest for future diagnostic strategies – rather, it was the capability to easily test patients across multiple locations and produce results on site in minutes.
It was not just COVID-19 rapid tests that hit the headlines in 2020. In July, Sky News reported, ‘the number of HIV self-testing kits [which included lateral flow] issued in London was 20% higher during the first eight weeks of lockdown than the same time last year’ and ‘orders in some London boroughs rose by over 70%’.
Rapid test usage will not stop post-pandemic
The pandemic has taught us the value of mass screening and illustrated how getting a broad picture of the status of disease infection as easily and quickly as possible contributes to setting appropriate and targeted response strategies. Various diagnostics methods played their role during the pandemic response. Extensive media coverage was given to swab testing, a method where samples are collected at testing centres or via self-testing before being sent to laboratory for a confirmatory result via PCR (Polymerase Chain Reaction). Testing companies worked diligently alongside logistics companies, who also scaled up their services, to ensure patient samples were swiftly delivered to the labs to enable the fastest possible results and turnaround times.
The response to the SARS-CoV 2 pandemic suggests that laboratory methods may not be the sole solution for infectious disease testing in the future, especially where the need for results is time critical due to a disease’s short incubation or latency period: Ebola being one example.
Accurately producing and reporting results on the same day – for all infectious diseases, irrespective of their incubation period – not only delivers a patient-centric response, but could potentially also offer resourcing benefits through reducing the number of people needed to process and interpret a result.
It is also important to understand the dynamics and demographics of global populations, to demonstrate fully why the use of rapid tests is beneficial for future testing programmes. It is projected that throughout the world, the number of people aged 60 or above will be approximately 1.4 billion in 2030 and 2.1 billion in 2050. When infectious disease risks are coupled with the fact that ageing populations, with ever greater numbers of chronic ailments and autoimmune conditions, lead to an increase in demand for primary care, patient care systems will be under greater pressures and will need to be responsive and deliver effective diagnostics quickly. A potential release of the ‘pressure value’ with rapid tests may be required as the burden on the health economics in both private insurance systems and centralised public health continues to grow.
Appointment and treatment backlogs owing to delays occasioned by COVID-19 could potentially have a long-lasting effect. In October 2020, several UK media outlets highlighted long delays in routine blood testing services in Barking and Dagenham, Havering, and Redbridge. If this happened in London boroughs, did it happen in phlebotomy departments throughout the UK? Meanwhile, considering 1,272,300 patients were waiting for a ‘key diagnostic test’ (all types of diagnostics) across the UK at the end of September 2020, an increase of 249,300 from September 2019, the ripple effect into budgeting and resource management may be far-reaching.
The speed and ease of use of rapid tests could potentially alleviate the pressures on primary care diagnostics by offering a testing solution that does not need several departments to deliver a result. The public have had their eyes opened to the benefits of rapid tests; and this will lead to an increase in demand, with some patients expecting test results to be delivered quickly or immediately. In turn, doctors, by their very nature, will want to supply fast and efficient diagnosis to deliver the best service.
Abingdon Health feels using rapid tests as a part of ‘best practice’ approach could benefit diagnostics services in the future. In lateral flow testing, world healthcare systems have an appropriate tool to respond to the next global outbreak but more appropriately have an intuitive solution to help stop local outbreaks becoming a national or worldwide problem.

Precision medicine, decentralisation, and data
Lateral flow technology is not one-dimensional and can act as a companion diagnostic to support patient-centric solutions or precision medicine strategies: initiatives designed to tailor treatment and patient management to the individual in support of the best outcomes, thus avoiding the unnecessary use of treatments and resources.
Rapid tests can support drug or vaccine clinical trial efficacy by helping to confirm the presence of biomarkers. Fast monitoring of an immune response or known side effects in any location means clinical trial managers can build a validation dataset quickly.
Another interesting aspect is how rapid tests may have the potential to help clinical trial patient recruitment. 70% of potential clinical trial patients live more than two hours’ travel away from their nearest study centre. The impact of trial participation on a patient’s life is significant when they must regularly visit trial clinics, especially in the cases of patients with mobility or chronic health issues. This statistic could also go some way towards explaining why 85% of all clinical trials fail to recruit enough patients. It is feasible that testing biomarkers with an easy and portable rapid test that fits in and around a patient’s lifestyle, while allowing professionals to gain the results quickly, could have a positive impact on future clinical trials.
This ease of testing response markers could also benefit monitoring patients once a drug or vaccine has been approved for general use, enabling clinicians to regularly assess how a patient is responding.
Several of the COVID-19 vaccines in development and production are designed to produce IgG antibodies to the SARS-CoV-2 full trimeric spike protein1, 2 the type of antibodies produced as immunity develops. There is a possibility rapid tests that detect these specific IgG antibodies, such as Abingdon Health’s AbC-19™ Rapid Test, could complement vaccinations by regularly testing individuals for the purpose of confirming the desired immune response or supporting evidence gathering for validating the optimum dose.
Furthermore, as COVID-19 research continues it is possible rapid tests could regularly test positive COVID-19 patients or vaccinated individuals, over months or years, in order to gather evidence for better understanding how long immunity markers stay present in the body.
In another area of diagnostics, the creation of isothermal amplification molecular tests, such as Recombinase Polymerase Amplification (RPA) and loop mediated isothermal amplification (LAMP), has allowed molecular testing to take place in multiple environments with limited resources. However, molecular testing still requires a final step of nucleic acid detection: a method traditionally carried out in a laboratory using expensive equipment and relying on postal services to deliver samples. A complementary rapid test can negate the use of the traditional method and support a true decentralised, point of care molecular testing solution. So, when combining molecular testing with portable nucleic acid detection rapid tests, the two technologies become a powerful partner in creating the opportunity to deploy in-field or point-of-care (POCT) molecular testing to multiple locations. In addition, the ability to combine rapid tests with connected data platforms via readers acts as another value-added feature of lateral flow.
Diagnostics data is an increasingly important commodity for gaining insights into accurately guiding patient treatments or aiding epidemiology studies. Combining smartphone apps, such as Abingdon Health’s AppDx®, with rapid tests allows real-time data to be captured in situ via the phone’s camera and shared via readily available connectivity technology such as Wi-Fi or Bluetooth. Collating data in this way means treatments, response strategies, improvements or solutions are based on real-time data.
In the following hypothetical scenario, it makes it easier to contextualise why rapid tests alongside connected data capture is valuable:
Several individuals are being tested for a disease – say norovirus, malaria, or influenza, to give a few examples – in multiple medical centres across a city or region; and there is no known outbreak. The rapid test results are produced during the appointments, recorded on a smartphone app and shared immediately to a central data hub, accessible by key stakeholders. A spike in positive cases in an unexpected time frame is detected within the central data hub and a pre-set algorithm triggers an automated alert to inform authorities of a potential health threat.
Without the rapid results and the instant connected data transfer, the response in this scenario could be different.
Furthermore, combine lateral flow’s data capture capabilities with the companion and complementary diagnostics examples given earlier and the technology becomes an even more powerful tool in diagnostics. But it does not stop there. As healthcare policymakers start to consider self-testing more and more, lateral flow is well placed for this; pregnancy is testament to its feasibility, as is the HIV self-testing mentioned earlier in the article.
Manufacturing for future demand
In the USA alone in 2020, all lateral flow clinical testing was valued at approximately $3bns. The compound annual growth rate (CAGR) for the whole lateral flow market is predicted to be 4.5% by 2025; applying 4.5% CAGR to just USA-based lateral flow clinical testing and coupling this prediction with the external market drivers, it is easy to see why this article predicts the use of lateral flow will be more common.
Demand for rapid test products is being answered by manufacturers. Of course, during the COVID-19 pandemic, the supply chain mobilised in response to an international ‘call to arms’: material and equipment suppliers and established rapid test manufacturers with expertise and the necessary infrastructures came forward to support the cause; even companies with little or no previous experience in rapid test manufacturing joined in the humanitarian fight. But 2020 was only the start for rapid test manufacturers responding to increasing requests for lateral flow.
Production facilities are expanding as specialist rapid test manufacturers look to accommodate future demand. Abingdon Health’s expansion plans, which commenced in 2019 and accelerated in 2020, led to an increase in its manufacturing footprint with additional sites and the addition of new semi-automated and automated lines alongside an increase in its quality assurance and regulatory affairs capacity.
It is feasible that the number of new rapid test manufacturers will grow and that these manufacturers will play an important role in future by servicing various proportions of demand. However, it is highly likely that those new to lateral flow or looking for a new or second manufacturer will seek a ‘safe pair of hands’ from established manufacturers who offer experience and expertise alongside a security of supply.

Conclusion
A handful of organisations worldwide were spreading the good word of rapid tests and their potential in global diagnostics long before the coronavirus crisis. However, it is possible for future pandemic or non-pandemic situations, the use of rapid tests will be considered more readily.
Self-isolation, social distancing and hand hygiene have become familiar habits; and these prevention tactics will be used for a long time. In the future, some policymakers may say self-isolation should be the ‘go-to’, alongside relying on more labour-intensive laboratory diagnostic methods. Is this the right approach? Would employers appreciate staff members being off work ‘just in case’ without a positive result? Would the self-employed appreciate loss of income because they are forced to stay at home ‘just in case’ while they wait for a result?
Rapid and accurate diagnosis technology is available and using the right tools is the key to deliver the best patient care while protecting the wider public and avoiding bumps in economic productivity.
The role of rapid tests in response to COVID-19 cannot be ignored. It is a shame it has taken a global health crisis to bring lateral flow rapid tests further up the agendas of more professionals and lay people. However, future generations may gain as a result, which is one very small consolation to come from the COVID-19 pandemic.
The many benefits of lateral flow in decentralised point-of-care testing offer the potential to contribute positively to people’s overall wellbeing. Deliver a negative result in minutes to someone who thought they might have a disease: no long anxious wait for the result. Conversely, a positive result means treatment can start there and then: the quick result has a positive impact on both physical and mental health.
This sentiment is already being realised throughout the world as lateral flow rapid tests become a household term. From a humanistic, commercial and resource management perspective the benefits of offering an easy-to-use fast screening tool, that can also be a companion or complementary diagnostic or combine with data platforms, is the reason why rapid tests may be in greater demand from now on.
References
- Staines, HM et al. Dynamics of IgG seroconversion and pathophysiology of COVID-19 infections. www.medrxiv.org/content/
- 1101/2020.06.07.20124636v2. Accessed 12 November 2020.
- Pfizer Vaccines. Behind the science: what is an mRNA vaccine? (25 August 2020) www.pfizer.co.uk/behind-science-what-mrna-vaccine. Accessed 12 November 2020.
Malcolm Briggs
Abingdon Health
info@abingdonhealth.com
www.abingdonhealth.com
This article is from issue 16 of Health Europa. Click here to get your free subscription today.






















