Introducing Otsuka Health Solutions’ award-winning Management and Supervision Tool (MaST) – the algorithm designed to reduce the burden on mental healthcare services.
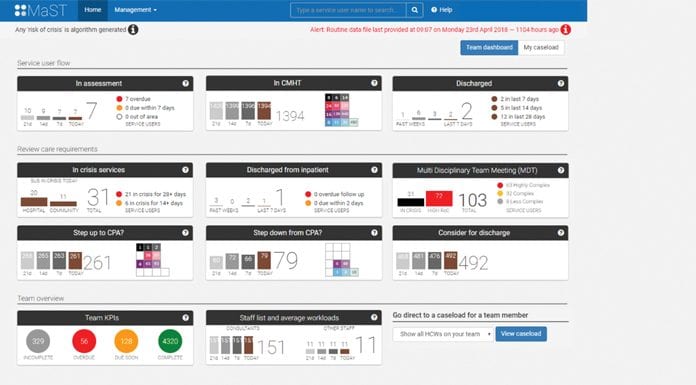
Mersey Care NHS Foundation Trust has launched Otsuka Health Solutions’ award-winning Management and Supervision Tool (MaST) across all of its Community Mental Health Teams. Using predictive analytics presented in an innovative dashboard, practitioners can now, at a glance, identify which service users might be at greatest risk of using crisis services and which might be ready to continue their recovery in the primary care sector. MaST allows the practitioner to prioritise their interventions and move to a preventative rather than treatment focused model of care.
NHS England’s Global Digital Exemplar (GDE) scheme has allowed both Mersey Care NHS Foundation Trust and fast follower, North West Boroughs NHS Foundation Trust to implement this technology and start to improve the digital systems available to their clinical teams for the long term.
Background
In the UK 1 in 4 people diagnosed with a mental health condition have reported waiting more than three months to see an NHS mental health specialist.1 Long waiting times have been found to generate a further deterioration in mental health, and broader social consequences, including divorce (36%), financial troubles (32%) and work problems such as job loss (34%).1
The increasing burden on mental health services along with important NHS England initiatives such as the Global Digital Exemplars (GDE) created an opportunity for NHS Mental Health Providers to rethink the way patient data is used in healthcare.2 Mersey Care NHS Foundation Trust has worked with OHS aiming to deliver safer care and an improved experience for service users and frontline staff.
OHS have developed the Management and Supervision Tool (MaST), a software platform which analyses data and uses predictive algorithms to inform healthcare staffs’ decision making based on service user needs and the likely resources required to support safe and effective care.
The technology
MaST uses a Risk of Crisis algorithm to identify those people who are most likely to require crisis services such as A&E, community crisis services or inpatient care. MaST can also be used to identify people who are at lowest risk of using crisis services and can hence be reviewed for potential discharge with support from other services for their continued recovery. This may ease patient flow, and free up resources for other people.3
OHS evaluate the effectiveness of the algorithm with formal reporting on the algorithm performance reviewed monthly. The Risk of Crisis analysis shows what proportion of uses of crisis services occur in a given proportion of service users (‘observations’) when ranked based on decreasing likelihood of such use as estimated by the risk algorithm. In Mersey Care, algorithm performance is evaluated monthly to ensure that between 70-75% of all crises from the caseloads come from the top 20% of service users identified by the Risk of Crisis Algorithm. Any variability in performance is addressed and improvements are made.4
In addition to the risk propensity cohorts, MaST assesses the complexity of service users based on factors including MAPPA (Multi-Agency Public Protection Arrangements), substance misuse and safeguarding concerns. MaST combines the Risk of Crisis quintiles with complexity ratings (high, medium or low) to create the MaST grid, which supports decision making by identifying cohorts of people who may require different care resources. For example, appropriateness for stepping up to a care programme approach (CPA) or stepping down from CPA, appropriateness for considering for discharge.
Engagement
The OHS team’s early engagement with clinicians, team leaders and frontline staff has a reciprocal theme. It is important that OHS are able to understand service delivery models and identify how MaST can support these, and it is important for staff to see parallels with the trust’s transformation agenda, and understand how MaST can support them to deliver this. In Mersey Care, this meant placing clinicians in the very centre of the project and allowing OHS staff to walk the floor to engage directly with staff about the struggles they experienced. From the outset Mersey Care recognised that to be successful, this needed to be a groundswell adoption as opposed to a top down delivery.
OHS uses a proven methodology to collaborate effectively with service users and staff, iterating the solutions to include users at every stage of the design process:
- Listening to care coordinators, medical staff and managers describe their experiences;
- Jointly developing and prioritising user stories;
- Adapting flexible components of the software; and
- Seeking feedback from end users and validating the data.
As a result of this approach, Mersey Care staff could visualise the benefits of the MaST system on working methods and caseload management with potential benefits in different settings as shown in the table below:3
Summary of benefits described by participants in Mersey Care’s evaluation of MaST3
Individual caseload management
- Greater transparency
- More appropriate allocation (caseload size/complexity)
- Enables reallocation of resources (e.g. staff sickness)
Supervision
- Prioritisation of workload (helping to manage staff stress)
- Focuses discussions to areas of need (objective overview)
- Less time trawling through notes, more time identifying problems
Multi-disciplinary team and stepped up care meetings
- Adds structure and focus to meetings, ‘leads’ the meetings
- Evidence basis for discussion, more objectivity, less subjectivity to decision making
- Prioritises time to those in greatest need
- Better planning (crisis intervention and discharge)
- Reduces emphasis on reflection (better done in other forums)
Now that MaST has been successfully launched into mental health services in England and is available for NHS organisations to buy through the Gov.uk digital marketplace, the OHS team have reflected upon the journey so far:
- The team have worked hard to put robust controls in place, complying with appropriate policies and processes of the healthcare organisation as well as their own internal polices with a programme of ongoing training and refresher sessions. These include policies such as information governance, confidentiality agreements, data protection and acceptable use policies.
- OHS introduced Mersey Care to an agile approach to development, meaning they had implemented and reviewed several iterations of MaST with a small group, before launching the solution across with the teams. The approach looked at how to alleviate barriers and enhance opportunities for positive change and engagement. Working in an agile way meant that the team could learn quickly and make adaptations as required to improve the experience for those using MaST.
- Working in true partnership with the NHS is essential. OHS needed front line staff and not just executives to support for the design, development, uptake and implementation of MaST. Key stakeholders and influencers were identified throughout the teams based on how they could help support change management within an organisation. It was notable that staff also self-selected into this role, offering their time and support with data validation, advocacy and supporting other colleagues to see its value.
Next steps for MaST include ongoing implementation across several mental health trusts in England along with an exciting development programme to refine and improve OHS’s existing analytics platform.
References
- https://www.bma.org.uk/news/media-centre/press-releases/2018/february/new-bma-research-unveils-blindspot-in-mental-healthcare
- https://www.england.nhs.uk/digitaltechnology/connecteddigitalsystems/exemplars/
- Data on File: The Healthcare Research Partnership: Evaluation of MaST System (Jan 2018)
- Data on File: Otsuka Health Solutions (OHS): Risk of Crisis Algorithm Analyses (2017-2019)
Caroline Gadd
Director
Otsuka Health Solutions
+44 (0)7826913269
cgadd@otsuka-europe.com
www.otsukahealthsolutions.com
This article has also appeared in Health Europa Quarterly Issue 11, which is available to read now.
























