Osteoporosis is the world’s most common bone disease; affecting approximately 200 million people globally,1 it results in more than 8.9 million fragility fractures each year, with about one in three women and one in five men over the age of 50 experiencing a fragility fracture in their lifetime.2
But with more people living longer, is enough being done to ensure those at risk of fragility fractures are being identified and adequately managed so they can enjoy fulfilling later lives?
People are living longer and, quite rightly, expecting more out of life in their later years. Between 2015 and 2030, the number of people in the world aged 60 years or over is projected to grow by 56% to 1.4 billion, and by 2050, the global population of older people is projected to more than double its 2015 size, reaching nearly 2.1 billion.3 According to the International Osteoporosis Foundation (IOF), the increase in fragility fracture incidence across six European countries (France, Germany, Italy, Spain, Sweden and the UK) alone between 2017 and 2030 is estimated at 23%.4
These fragility fractures have the potential to impose a significant burden on a person’s life, often making everyday activities such as eating, dressing, shopping or driving difficult.5 Those that suffer a hip fracture face reduced mobility, disability and loss of independence: a year after fracture 40% are not able to walk independently and 10–20% require long-term nursing care.6,7 Vertebral fractures can also place a large burden on the patient – leading to back pain, height loss, deformity, immobility and even reduced lung function.8,9,10 Unfortunately these are common fractures, occurring every 22 seconds worldwide in men and women over 50.11
While the physical implications are clear, a recent European survey of women living with osteoporosis by UCB, highlighted that osteoporosis isn’t just about broken bones – patients surveyed revealed that the condition makes them feel depressed (57%), vulnerable (61%), and isolated (27%).12
In addition to the human cost, fragility fractures cost health systems in the European Union €37 billion in 2010 and based on demographic changes, costs are predicted to double by 2050.1,13 The IOF reports that osteoporosis takes a huge personal and economic toll. In Europe, the disability due to osteoporosis is greater than that caused by cancers (with the exception of lung cancer) and is comparable or greater than that lost to a variety of chronic non-communicable diseases, such as rheumatoid arthritis and asthma.14
In women over 45 years old, osteoporosis accounts for more days spent in hospital than many other diseases, including diabetes, yet a higher priority is afforded to these conditions within health systems.15
Given the urgency of the situation and the impact of osteoporosis, learnings can, and should, be taken from other disease areas, such as diabetes. One way to enhance and individualise the care of patients with osteoporosis would be a treat-to-target approach much in the same way that people with diabetes are often set an HbA1c target.
Key learnings can also be taken in disease states where patients are educated on their current disease status, in addition to being informed on future risks and their implications, at the time of diagnosis. The introduction of the Fracture Liaison Services (FLS) in the United Kingdom in the late 1990s,16 addressed some of the challenges faced by those with osteoporosis who have already suffered a fracture. Whilst the IOF now records 225 FLS in over 35 countries,17 broader uptake of these services, coupled with a robust preventative treatment pathway, could mean an increase in patient care and a decrease in the burden the condition is putting on patients, the health systems and society as a whole. This is particularly relevant and imperative since ‘fracture begets fracture’, and worldwide only one in four patients who has suffered a fragility fracture Is currently evaluated and treated to decrease the risk of another fracture.
The ever-growing public health burden from osteoporosis and fragility fractures highlights the need to prioritise fragility fractures in healthcare systems immediately.4 Missing opportunities to respond to the first fracture is placing a burden on both the patient and healthcare systems more widely – to prevent personal and societal cost, it is essential to both recognise the underlying cause of fragility fractures, as well as acting to prevent a subsequent fracture. Fortunately, provisions such as the FLS have been shown to reduce the frequency of subsequent fractures, improve adherence to treatment and provide cost savings when correctly implemented.18,19,20,21,22,23 But action is needed such that the care that FLS afford become the standard.
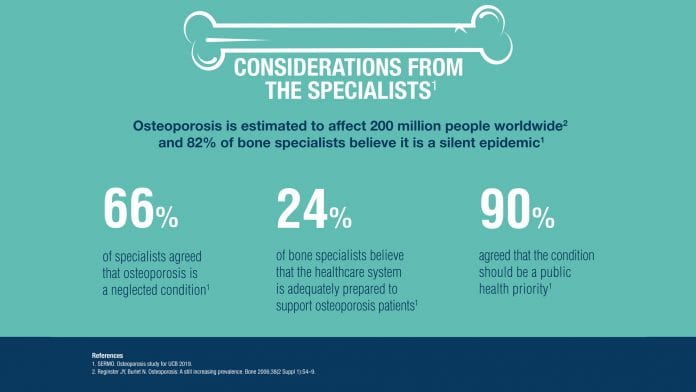
In a recent survey by UCB of healthcare professionals with a speciality in bone medicine,24 three quarters agreed that osteoporosis and fragility fractures should be given a higher priority than currently received within their health systems. 82% also said they believe that osteoporosis is a silent epidemic – and 24% felt the healthcare system is inadequately prepared to support osteoporosis patients. So, why isn’t osteoporosis receiving the attention it warrants?
Ultimately, a higher prioritisation needs to be given to osteoporosis identification, education and management. Osteoporosis and fragility fractures place an enormous burden on health systems and individuals across the globe. Healthcare professionals agree that a higher priority should be given to osteoporosis and fragility fractures if we are to reduce this burden, but at present these conditions are being overlooked and under prioritised.
We hope that with an increase in investment for osteoporosis and fragility research, innovation and education, we can collectively tackle the issues faced by those living with the conditions and support those HCPs who play a vital role in the patients’ journey in order to allow them to age healthily.
 Cesar Libanati
Cesar Libanati
Head of Medical Strategy
Bone
UCB
Cesar.Libanati@ucb.com
www.ucb.com
References
- Reginster JY, Burlet N. Osteoporosis: A still increasing prevalence. Bone 2006;38(2 Suppl 1):S4–9.
- Ström O, Borgström F, Kanis JA, et al. Osteoporosis: burden, health care provision and opportunities in the EU: a report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA). Arch Osteoporos 2011;6:59–155. doi:10.1007/s11657-011-0060-1.
- International Osteoporosis Foundation. IOF Compendium of Osteoporosis – First Edition.
- International Osteoporosis Foundation (IOF). Broken bones, broken lives: A roadmap to solve the fragility fracture crisis in Europe. [Online] Available at: http://share.iofbonehealth.org/EU-6-Material/Reports/IOF%20Report_EU.pdf. (Last accessed January 2020).
- Cooper C. The crippling consequences of fractures and their impact on quality of life. Am J Med 1997;103:12S–17S; discussion 17S–19S.
- International Osteoporosis Foundation. The Global Burden of Osteoporosis. What you need to know, Available at: https://www.iofbonehealth.org/sites/default/files/media/PDFs/Fact Sheets/2014-factsheet-osteoporosis-A4.pdf. Last accessed December 2019.
- Magaziner J, Simonsick EM, Kashner TM, et al. Predictors of functional recovery one year following hospital discharge for hip fracture: a prospective study. J Gerontol 1990;45:M101.
- Schlaich, C., Minne, H., Bruckner, T. et al. Reduced Pulmonary Function in Patients with Spinal Osteoporotic Fractures . Osteoporos Int 8, 261–267 (1998). https://doi.org/10.1007/s001980050063.
- Lips P, Cooper C, Agnusdei D, et al. (1999) Quality of life in patients with vertebral fractures: validation of the Quality of Life Questionnaire of the European Foundation for Osteoporosis (QUALEFFO). Working Party for Quality of Life of the European Foundation for Osteoporosis. Osteoporos Int 10:150.
- Pluijm SM, Dik MG, Jonker C, et al. (2002) Effects of gender and age on the association of apolipoprotein Eepsilon4 with bone mineral density, bone turnover and the risk of fractures in older people. Osteoporos Int 13:701.
- Vertebral fractures due to osteoporosis. [Online] Available at:http://worldosteoporosisday.org/sites/default/WOD-2018/Vertebral-Fracture-Factsheet_ENGLISH.pdf (last accessed January 2020).
- Data on file. Research Partners. Osteoporosis research for UCB, September 2019.
- Hernlund E, Svedbom A, Ivergard M, et. al. 10.1007/s11657-013-0136-1. 2013;8(1–2):136.
- Johnell O and Kanis JA (2006) An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int 17:1726.
- International Osteoporosis Foundation. Osteoporosis in the European Union in 2008: Ten years of progress and ongoing challenges (October 2008). Available at:http://www.iofbonehealth.org/sites/default/files/PDFs/EU%20Reports/eu_report_2008.pdf (last accessed February 2020)
- Bonanni S, et al. The Role of the Fracture Liaison Service in Osteoporosis Care. 2017;114(4):295–298.
- IOF Capture the Fracture: FLS Around The World Apply For Capture The Fracture Recognition. Available at:https://www.capturethefracture.org/fls-around-world-apply-capture-fracture%C2%AE-recognition . Last accessed December 2019.
- Boudou L, Gerbay B, Chopin F, et al. Osteoporos Int 2011;22(7):2099–106. (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6140089/#b9-ms114_p0295). Last accessed December 2019.
- Marsh D, Akesson K, Beaton DE, et al. IOF CSA Fracture Working Group. Osteoporos Int 2011; 22(7):2051–65.
- McLellan AR, Gallacher SJ, Fraser M, et al. Osteoporos Int 2003;14(12):1028–34.
- McLellan AR, Wolowacz SE, Zimovetz EA, et al. Osteoporos Int 2011;22(7):2083–98.
- Miki RA, Oetgen ME, Kirk J, et al. J Bone Joint Surg Am 2008;90(11):2346–53.
- Nakayama A, Major G, Holliday E, et al. Osteoporos Int 2016;27(3):873–879.
- SERMO. Osteoporosis study for UCB 2019.


























