
Dr Ghada Zoubiane and Georgiana-Simona Baciu of the International Centre for AMR Solutions explore the risks posed by antimicrobial resistance, as well as how to tackle drug-resistant infections.
Antimicrobial resistance (AMR) is one of the greatest threats to the health of humans, animals, crops and the environment. It is a One Health issue which affects societies and economies worldwide. In 2016, the World Bank estimated that by 2050, AMR could result in 28 million people living in poverty, a 7.5% decline in global livestock production, a 3.8% reduction in global exports and $1tn in additional healthcare costs1. The World Health Organization (WHO) has classified AMR in the top 10 threats to global health.
Drug-resistant infections threaten global efforts to achieve many of the United Nations’ Sustainable Development Goals (SDGs)2; and have gained significant visibility on the global political and public health agendas in recent years. From a human health perspective, a world without effective antimicrobials such as antibiotics would be an end to healthcare as we know it. The independent O’Neill Review estimated that 10 million people will die due to AMR by 2050 if nothing is done3, up to nine million of whom will be in low and middle-income countries (LMICs).
AMR and COVID-19
Currently, the world is rightly focused on tackling COVID-19. At the same time, this pandemic is only a foretaste of what AMR could mean to the world without appropriate interventions. COVID-19 has intensified the problem of AMR due to extensive and inappropriate antimicrobial and biocide use.
In many countries, due to lack of capacity to test COVID-19 patients for bacterial infections, there is a tendency to prescribe broad-spectrum antimicrobials to hospitalised patients prophylactically and/or empirically4 to ensure that any existing co-infections do not aggravate their symptoms. At the same time, the overwhelming number of patients visiting hospitals means that there is closer proximity between patients on hallways and in crowded hospital rooms. This potentially leads to more exposure and faster spread of bacteria; and with vaccination programmes heavily curtailed in many countries5, this has potentially increased infections and subsequently antimicrobial use and resistance. Moreover, COVID-19 brought a sharp increase in the use of disinfectants. Biocides contained in hand sanitisers and household disinfectants have been reported to potentially affect antibiotic resistance6.
On the other hand, one cannot disregard the converse scenario, where changes in health seeking behaviour and non-pharmaceutical interventions such as of wearing masks, physical distancing and hand washing/hygiene may decrease the incidence of all infections especially in the community, reducing the need for antibiotics and thereby reducing selection pressure for AMR. Nevertheless, even with these potentially positive effects, AMR continues to be an imminent threat to global health. The consequences of the COVID-19 pandemic demonstrate the need for continued and intensified efforts to mitigate the AMR pandemic and transform global policies into concrete actions on the ground.
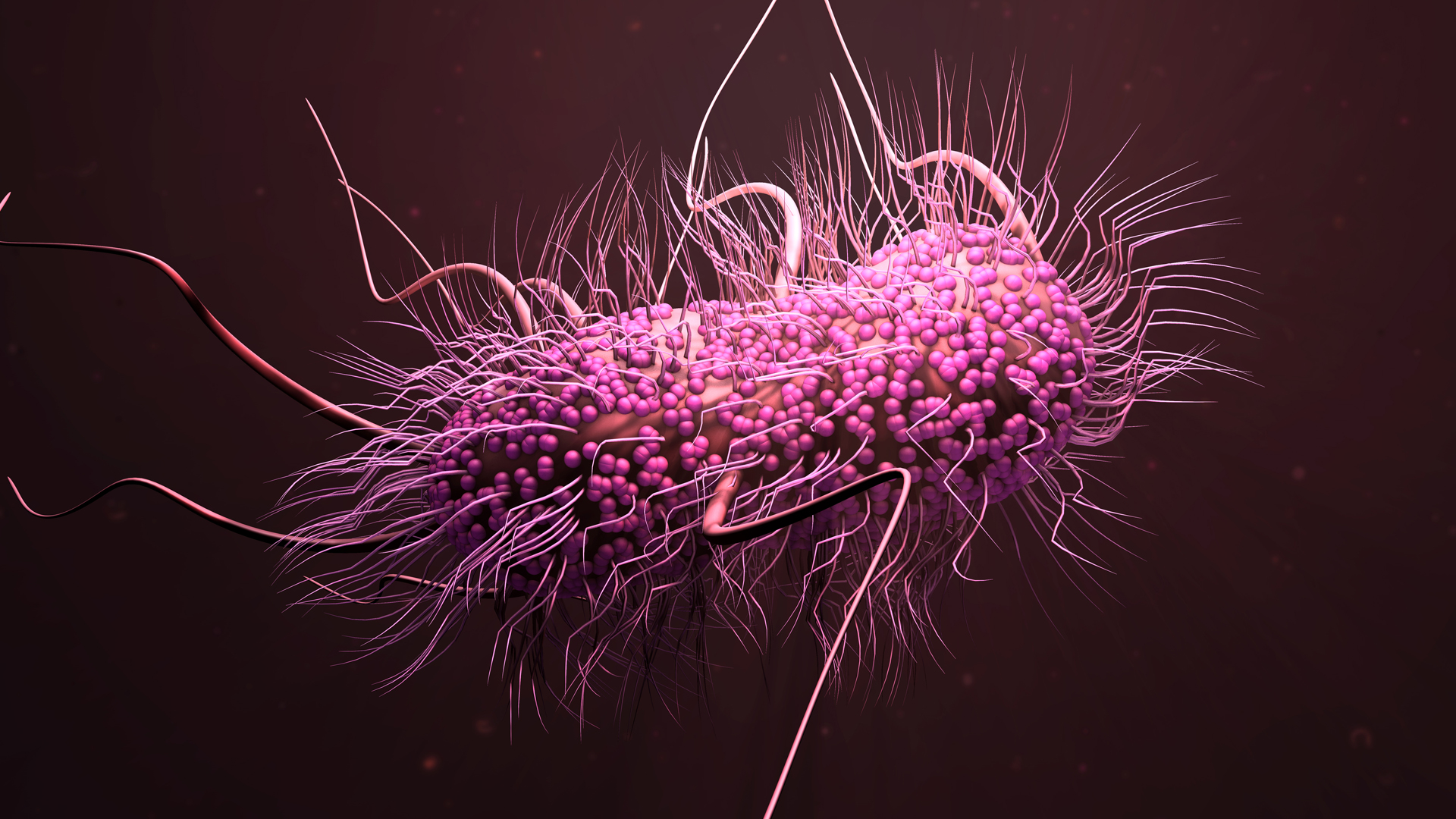
There is no face for drug-resistant infections, a large group of invisible, untraceable threats, which quietly take over the world and for which testing is not as easy to perform as for one specific virus like COVID-19. In comparison with COVID-19, which has transformed the world very visibly from one week to the next, the spread of AMR leading to increasing number of hard-to-treat infections comes in small increments. Currently, most people – especially in the Western world – are either never or only rarely confronted directly with the severe consequences of infections due to multi-resistant bacteria. It is estimated that resistant bacteria presently cause more than 700,000 deaths every year, more than a third of the deaths ascribed to COVID-19. It is projected that this number will constantly rise, impacting morbidity, mortality and the economy far greater than COVID-19, all while the world has limited perception of being hit by a second pandemic – hence the term ‘the silent pandemic’.
When the day comes that current antibiotics become ineffective against most infections, the world will have to ‘put a face to the name’, though by then it will be too late. That is why the time to act is now, to prevent infections in the first place, curb the spread of AMR, develop new types of medication and protect the antibiotics we currently have.

Closing the gap between policy and practice in LMICs
By November 2020, 143 countries had developed National Action Plans (NAPs) for the mitigation of AMR7. This is a very positive development that stems from an increase in global awareness of the threat of AMR and policies aiming to mitigate it. However, implementation remains a challenge, particularly in LMICs which require substantial development assistance to implement their NAPs at scale, together with whole-of-government ownership to ensure long-term sustainability of these investments at national level.
While there is currently a growing body of evidence on effective interventions to tackle AMR, the majority of it has been developed in high-resource, high-income countries and cannot be directly translated to LMICs which have different settings and would require more tailored context-specific solutions. There is a need for intervention and implementation research that aims at developing and testing solutions tailored to the specific context in which they are to be used. Such solutions will require strong partnerships between government ministries and a range of national and regional stakeholders, including but not limited to research organisations, civil societies, and private and non-governmental sectors.
ICARS: an implementation research partnership
A Danish-founded organisation, ICARS’ mission is to enter into funded partnerships with LMICs to advance the implementation of their National Action Plans. Specifically, ICARS partners with LMICs to develop and test context-specific solutions for AMR mitigation, translate existing evidence into action and, as part of these activities, support targeted capacity and capability building in the country. ICARS further advocates for the need for intervention and implementation research as a means to deliver on the NAPs. The organisation works with implementation partners and builds on existing national and international initiatives to expand the scale and scope of the AMR response, and boost investment and collaboration across sectors.
A unique approach
ICARS brings a different approach to tackling AMR – a funded partnership, collaborating with the country to co-develop evidence-based, context specific, cost-effective and sustainable solutions to combat AMR, advancing each country’s individual NAP implementation.
Each country is different both in its approach to tackling AMR and in the type of issues that accelerate AMR at a local level. National commitment is crucial to ensure uptake and translation of interventions into large scale sustainable action including national policies, programmes and practices. By combining a top-down and bottom-up approach, ICARS secures commitment and ownership from the relevant government ministry or ministries, while rooting the projects in scientific research conducted at local and national levels.
The ICARS strategy
ICARS’ strategy is based on four interconnected pillars. These ensure that the action against AMR is targeted and multi-directional, leading to long-term behaviour change.
- Pillar 1: co-develop and test context-specific solutions for AMR mitigation, in partnership with LMIC ministries who lead their intervention and implementation;
- Pillar 2: translate existing evidence into action by reviewing the existing evidence and where appropriate engaging with and facilitating dialogue between the research community and the relevant ministries to identify barriers and enablers for the implementation of such solutions;
- Pillar 3: Advocate for intervention and implementation research as an important tool to tackle AMR by engaging with national and international partners to raise awareness and mobilise support for One Health intervention and implementation research nationally and internationally to mitigate AMR; and
- Pillar 4: support targeted capacity and capability of AMR in LMICs, by working with partners to expand the implementation of existing successful capacity building tools and provide implementation research training, for the benefit of professionals in partnering LMICs.
Evidence into practice
ICARS was formally established in May 2019. Since then, it has begun working on four projects to tackle AMR in partnership with the governments of Vietnam and Georgia, while establishing collaborations with implementation partners such as WHO, ReAct and JPIAMR. ICARS is in discussion with several other LMICs committed to tackling AMR. ICARS will become an independent organisation at some point this year. While currently being fully funded by the Danish government, other countries and foundations are invited to become Founding Members over the next two years.
References
1 World Bank (2017). Drug-Resistant Infections. A Threat to Our Economic Future.
2 United Nations Interagency Coordination Group on Antimicrobial Resistance (2019). No Time to Wait: securing the future from drug-resistant infections.
3 Jim O’ Neill (2016). Tackling Drug-Resistant Infections Globally: final report and recommendations. Review on Antimicrobial Resistance.
4 Rawson TM, Moore LSP, Zhu N, Ranganathan N, Skolimowska K, Gilchrist M, et al. (2020) Bacterial and fungal co-infection in individuals with coronavirus: a rapid review to support COVID-19 antimicrobial prescribing. Clinical Infectious Diseases.
5 Abdu A. Adamu, Rabiu I. Jalo, Desire Habonimana, Charles S. Wiysonge (2020), COVID-19 and routine childhood immunisation in Africa: Leveraging systems thinking and implementation science to improve immunisation system performance, International Journal of Infectious Diseases no. 98, pp 161-165
6 United Nations Environment Programme (2017), Frontiers 2017: Emerging Issues of Environmental Concern.
7 The World Health Organization
Dr Ghada Zoubiane PhD
Head of Partnerships and Stakeholders Engagement
Ms Georgiana-Simona Baciu MSc
Communications Officer
International Centre for AMR Solutions
www.icars-global.org
This article is from issue 16 of Health Europa. Click here to get your free subscription today.
























