
Matti Vartiainen from Ainone discusses a pilot study designed to identify balance quotient values for the baseline of athletes’ performance.
The ability to maintain postural control is determined by main input from visual, vestibular, and somatosensory systems (Gurley, Hujsak, & Kelly, 2013). Following concussion, communication between these sensory systems can be disrupted causing postural instability (Guskiewicz, 2001). Because balance and gait abnormalities are frequent after sport-related concussion (SRC) (Guskiewicz, Ross, & Marshall, 2001; Khurana & Kaye, 2012) sensomotor and balance testing is an important part of concussion evaluation, particularly in the acute stage (Broglio & Puetz, 2008; Davis, Iverson, Guskiewicz, Ptito, & Johnston, 2009; Eckner, Kutcher, & Richardson, 2010; Harmon et al., 2013; Khurana & Kaye, 2012; Mayers & Redick, 2012; McCrory et al., 2009; McCrory et al., 2017a; Sosnoff, Broglio, & Ferrara, 2008).
Multidomain sideline evaluation tools have been developed, including tests of vestibular-ocular function. Akhand and colleagues (2019) recently stated that ocular motor changes in performance after concussion reflect generalised neurophysiologic changes can affect a variety of cognitive processes. (Akhand et al. 2019). Balance deficits are mainly reported to resolve in three to seven days after concussion (Guskiewicz et al., 2001; McCrea et al., 2005), but recent evidence following concussion identified, using instrumented measurement, lingering impairments for at least one month (Buckley et al. 2016).
Balance control
Balance tests are normally conducted using stop-watch and error grading, but the test positions used in sport-related concussion evaluation have also been used in computerised balance testing in different clinical applications, such as hearing-impaired children (De Kegel et al., 2011), elderly falls (Howcroft, Lemaire, Kofman, & McIlroy, 2017), and multiple sclerosis (Kalron, 2017). Computerised force plates offer more precise and objective measurement of balance performance. However, when computerised force plates are used it is difficult to compare results across studies using different devices. Common nominators, such as potentially the Balance Quotient (BQ), are needed.
The Clinical Test of Sensory Integration for Balance (CTSIB), the Balance Error Scoring System (BESS), and the Sensory Organization Test (SOT) are widely used tests for balance assessment after concussion (Guskiewicz, 2001). CTSIB and BESS assesses static balance with eyes closed on three stances on either hard or soft surface and can be done in sideline, while SOT alters the available somatosensory or visual information and uses a technical force plate to measure the ability to minimise postural sway (Guzkiewicz, 2001; Giza et al., 2013; Harmon et al., 2013; McCrory et al., 2013). In addition to static balance, dynamic balance, gait and rhythmic coordination have also been found to be impaired following traumatic brain injury (Basford et al., 2003; Rinne et al., 2006).
Romberg test and balance quotient
The traditional Romberg test is also frequently used as a part of concussion assessment (Murray, Salvatore, Powell, & Reed-Jones, 2014). The Romberg test has been reported as quick tool and future prospect tool of recognising early Alzheimer stage (Gras et al. 2015) or mass evaluation tool for elderly fall risk evaluation (Gallamini et al. 2021). The influence of eye closing on stability can be expressed using the Romberg’s quotient, RQ (Van Parys & Njiokiktjien 1978; Dornan, Fernie, & Holliday, 1978; Morioka, Okita, Takata, Miyamoto, & Itaba, 2000; Le & Kapoula, 2008; Kapoula, Gaertner, Yang, Denise, & Toupet, 2013). The Romberg test is conducted with the feet together and with the eyes open and closed, and the result of RQ is the relative difference between those tests.
The feasibility of a computerised platform balance test and a calculated Romberg Quotient in acute recognition of concussion have been evaluated by Vartiainen et al. (2017). The Romberg test performance in four different conditions was evaluated at baseline and significant interactions between the visual and the somatosensory inputs was found. All sway parameters derived from the computerised balance board showed the change from the easiest (hard surface, eyes open) to the most difficult (soft foam, eyes closed) condition. The significant interaction between conditions supports the use of RQ, the ratio between eyes closed and eyes open, to study the effect of somatosensory conditions on postural stability. To conclude, alternating between different visual and/or somatosensory conditions in balance testing brings out the effect of concussions.
RQ is easy to calculate regardless of the measurement systems or scales and can be used as a valid tool in sport concussion measurement (Vartiainen et al. 2017). In a similar perspective of relative difference, when measuring balance control without visual input it has been stated that measuring sway in postural stability in standing on one leg, eyes open and closed conditions are suitable in the rehabilitation process of knee injuries (Lehmann et al. 2015).
The aim
The aim of this pilot study was to identify BQ values for the baseline of athletes’ performance in SCAT5/BESS (Echemendia et al. 2017) error calculation and physiotherapist’s visual/qualitative scoring system compared to effects of different visual and somatosensory conditions during balance testing in similar postures measured with sway in Ainone Balance® mobile application and Movesense sensor for balance measurement (Class I medical device/MDD).
Protocol
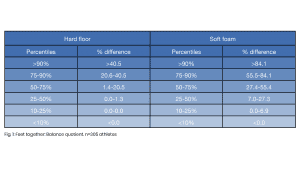
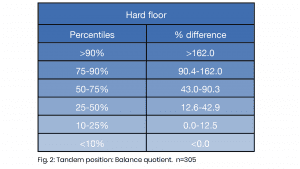
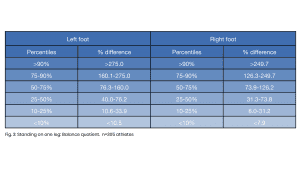
Balance tests were administered at baseline in between 2019-2021 to 305 healthy 18–40-year-old high elite athletes. The balancing postures were conducted similarly from SCAT5/BESS evaluation: standing feet together (Romberg position), tandem, and standing on one leg. All tests were conducted in 10 seconds on a hard and soft floor, eyes open and closed. Sway was measured with Ainone Balance (10 seconds). The percentiles were used as reference values. A relative balance change in Romberg test is called RQ (Van Parys & Njiokiktjien 1978), therefore the balance quotient was assessed by calculating the ratio between eyes open, and eyes closed parameters in all three stance conditions. Balance quotient was computed for sway length.
Results
Sway varied with the change in both somatosensory and visual conditions. The increase from eyes open to eyes closed condition was larger on more difficult conditions. As presented in Fig 1, the balance quotient between eyes open closed in bipedal stance/feet together. For example, if the sway length increases over 40.5% (hard) or 84.1% (soft), the BQ represents unusually low score. In Fig. 2, when the score in tandem position increase over 162.0% when eyes closed the result is an unusually low score. When standing on one leg, BQ over 249.7% on the right and 275.0% left represents an unusually low score (see Fig 3.)
Conclusion
The report represents balance quotient score in accordance with professional error/qualitative way (SCAT5/BESS) used in Ainone Balance sway measurement. These results give normative guidelines for BQ scores. In the future, these kinds of relative changes could be the value indicating the change after concussion and somatosensory integration problems as they have been studied regarding to RQ in pilot study of Vartiainen et al. (2017) and recommended to be a tool to discriminate elderly fallers (Howcroft et al., 2017).
This is a preliminary report of the use of balance quotient in process of balance evaluation and the use of concussions and can be conducted alongside with BESS error scoring and Ainone Balance sway measurement.
More study is needed but, measuring and analysis of BQ could be an be a way to differentiate balance system deficits in sports alongside to holistic evaluation process. The sway measurement is an objective way to evaluate performance difficulties and aiming towards a better recognition of concussions.
References
- Broglio, S. P., & Puetz, T. W. (2008). ‘The effect of sport concussion on neurocognitive function, self-report symptoms and postural control: A meta-analysis’. Sports Med, 38, 1, 53-67
- Gallamini, M.; Piastra, G.; Lucarini, S.; Porzio, D.; Ronchi, M.; Pirino, A.; Scoppa, F.; Masiero, S.; Tognolo, L. ‘Revisiting the Instrumented Romberg Test: Can Today’s Technology Offer a Risk-of-Fall Screening device for Senior Citizens? An Experience-Based Approach’. Life 2021, 11, 161 https://doi.org/10.3390/life11020161
- Akhand, O., Rizzo, J.R., Rucker, J.C., Hasanaj, L., Galetta, S.L., Balcer, L.J. (2019). ‘History and Future Directions of Vision Testing in Head Trauma’. J Neuro-Ophthalmol, 39(1), 68-81Davis, G. A., Iverson, G. L., Guskiewicz, K. M., Ptito, A., & Johnston, K. M. (2009). ‘Contributions of neuroimaging, balance testing, electrophysiology and blood markers to the assessment of sport-related concussion’
- Buckley, T.A., Oldham, J. R., Caccese, J. B. (2016). ‘Postural control deficits identify lingering post-concussion neurological deficits’. J Sport Health Sci, 5(1), 61-69
- De Kegel, A., Dhooge, I., Cambier, D., Baetens, T., Palmans, T., Van Waelvelde, H. (2011). ‘Test-retest reliability of the assessment of postural stability in typically developing children and in hearing impaired children’. Gait Posture, 33, 679-685
- Dornan, J., Fernie, G. R., Holliday, P. J. (1978). ‘Visual input: its importance in the control of postural sway’. Arch Phys Med Rehabil, 59, 586–591
- Eckner, J. T., Kutcher, J. S., & Richardson, J. K. (2010). ‘Pilot evaluation of a novel clinical test of reaction time in national collegiate athletic association division in football players’. J Athl Training, 45(4), 327-332
- Gurley, J. M., Hujsak, B. D., & Kelly, J. L. (2013). ;Vestibular rehabilitation following mild traumatic brain injury’. NeuroRehabil, 32(3), 519-528 doi:10.3233/NRE-130874
- Guskiewicz, K. M. (2001). ‘Postural stability assessment following concussion: One piece of the puzzle’. Clin J Sport Med, 11(3), 182-189 doi:10.1097/00042752-200107000-00009
- Guskiewicz, K. M., Ross, S. E., & Marshall, S. W. (2001). ‘Postural stability and neuropsychological deficits after concussion in collegiate athletes’. J Athl Train, 36(3), 263-273
- Gras LZ, Kanaan SF, McDowd JM, Colgrove YM, Burns J, Pohl PS. ‘Balance and gait of adults with very mild Alzheimer disease’. J. Geriatr. Phys. Ther. 2015 Jan-Mar;38(1):1-17
- Harmon, K. G., Drezner, J. A., Gammons, M., Guskiewicz, K. M., Halstead, M., Herring, S. A., Kutcher, J.S., Pana, A., Putukian, M., Roberts, W.O. (2013). ‘American medical society for sports medicine position statement: Concussion in sport’. Br J Sports Med, 47(1), 15-26 doi:10.1136/bjsports-2012-091941
- Howcroft, J., Lemaire, E.D., Kofman, J., McIlroy, W.E. (2017). ‘Elderly fall risk prediction using static posturography’. PLoS ONE, 12(2), e0172398
- Kalron, A. (2017). ‘The Romberg ratio in people with multiple sclerosis’. Gait & Posture 54, 209–213
- Kapoula, Z., Gaertner, C., Yang, Q., Denise, P., Toupet, M. (2013). ‘Vergence and Standing Balance in Subjects with Idiopathic Bilateral Loss of Vestibular Function’. PLoS ONE, 8(6), e66652 doi:10.1371/journal.pone.0066652
- Khurana, V. G., & Kaye, A. H. (2012). ‘An overview of concussion in sport’. Journal of Clin Neurosci, 19(1), 1-11 doi:10.1016/j.jocn.2011.08.002
- Lê, T.T., Kapoula, Z. (2008). ‘Role of ocular convergence in the Romberg quotient’. Gait Posture, 27, 493-500
- Lehmann T, Paschen L, Baumeister J. ‘Single-Leg Assessment of Postural Stability After Anterior Cruciate Ligament Injury: a Systematic Review and Meta-Analysis’. Sports Med Open. 2017 Aug 29;3(1):32 doi: 10.1186/s40798-017-0100-5. PMID: 28853022; PMCID: PMC5574832
- Mayers, L. B., & Redick, T. S. (2012). ‘Clinical utility of ImPACT assessment for postconcussion return-to-play counseling: Psychometric issues’. J Clin Exp Neuropsychol, 34(3), 235-242
- McCrory, P, Feddermann-Demont, N, Dvořák, J, Cassidy, J.D., McIntosh, A., Vos, P.E., Echemendia, R.J, Meeuwisse, W., Tarnutzer, A.A. (2017) ‘What is the definition of sports-related concussion: a systematic review’. Br J Sports Med, 51, 877-887
- McCrory, P., Meeuwisse, W., Johnston, K., Dvorak, J., Aubry, M., Molloy, M., & Cantu, R. (2009). Consensus statement on concussion in sport: The 3rd international conference on concussion in sport held in Zurich, November 2008. British Journal of Sports Medicine, 43(1), i76-i84 doi:10.1136/bjsm.2009.058248
- McCrea, M., Barr, W. B., Guskiewicz, K., Randolph, C., Marshall, S. W., Cantu, R., Onate, J.A., Kelly, J. P. (2005). ‘Standard regression-based methods for measuring recovery after sport-related concussion’. Journal of the International Neuropsychological Society, 11(1), 58-69
- Morioka, Okita M, Takata Y, Miyamoto S, Itaba H. (2000). ‘Effects of Changes of Foot Position on Romberg’s Quotient of Postural Sway and Leg Muscles Electromyographic Activities in Standing’. J Jpn Phys Ther Assoc, 3:17–20
- Murray N., Salvatore A., Powell D., Reed-Jones R. (2014). ‘Reliability and Validity Evidence of Multiple Balance Assessments in Athletes With a Concussion’. J Athl Training, 49(4), 540–549 doi: 10.4085/1062-6050-49.3.32
- Sosnoff, J. J., Broglio, S. P., & Ferrara, M. S. (2008). ‘Cognitive and motor function are associated following mild traumatic brain injury’. Exp Brain Res, 187(4), 563-571 doi:10.1007/s00221-008-1324-x
- Van Parys, J., Njiokiktjien, C.H. (1978). ‘Romberg’s sign expressed in a quotient’. Agressologie, 17(3): 95 -100
- Vartiainen, M, Holm, A, Koskinen, S, Hokkanen, L. (2017). ‘The feasibility of Romberg quotient in assessment of balance after sport concussion’. British Journal of Sports Medicine. 51. A57.3-A58 10.1136/bjsports-2016-097270.150
This article is from issue 19 of Health Europa Quarterly. Click here to get your free subscription today.

























