
Discover the SCUBY project, the mission of scaling up integrated care for diabetes and hypertension in Cambodia, Slovenia and Belgium.
The University of Antwerp’s Josefien Van Olmen discusses how the SCUBY project will improve care for patients with type 2 diabetes and hypertension while helping to reduce health inequalities.
Many countries struggle to find the best way to treat hypertension (HT) and type 2 diabetes (T2D). As a result, many patients receive suboptimal care, especially the vulnerable groups in society. The SCUBY project addresses this important societal issue by examining the scale-up of existing evidence-based interventions for the control of T2D and/or HT.
It is innovative because it compares different scale-up strategies for a contextualised common intervention package, thereby generating knowledge of the scale-up processes themselves. The proposal develops, implements and assesses roadmaps for the scale-up of the integrated care package for T2D and HT, in three different types of countries:
- A low-middle-income country (LMIC) with a developing health system
- A former socialist high-income country (HIC) with a still rather centralised health system
- A Western European federal country with a decentralised system.
These roadmaps will accelerate scale-up and contribute to sustainable coverage of T2D and HT interventions for more people in each country. The implementation and evaluation of the three roadmaps, one per country, will generate new knowledge on how to scale up integrated care for T2D and HT in diverse contexts.
The challenge of scaling up diabetes and hypertension care
The global prevalence of 9% for T2D and of 31.1% for HT reflects the dominance of these two conditions in the global burden of disease.1-3 Effective interventions for prevention, detection, treatment and control of both conditions are available but do not reach all people in need. As a result, T2D and HT are not well controlled, which increases the burden of their complications and people die prematurely. Figures show that 28.4% of people with HT in HICs and only 7.7% of people with HT in LMICs are well controlled.3 Vulnerable populations, in all contexts, are most affected. Scale-up of effective interventions should therefore specifically focus on LMICs and on vulnerable populations in other contexts, also HICs. Effective treatment for people who have HT and/or T2D exists and is cost-effective.4
An integrated care package
An integrated care package with five components is the core of the SCUBY project:
- Identification of people with HT and/or T2D
- Subsequent treatment in primary care services
- Health education
- Self-management support to patients and caregivers
- Collaboration between caregivers.
This package is endorsed by WHO recommendations and guidelines and has been shown to improve quality of care and improve health outcomes.5,6
Despite the existence of good practices, countries lag behind in their scaling up. There is a knowledge gap on how to get the health systems implementing the integrated care package, for instance on task division among health workers, on collaboration between community organisations and healthcare organisations, and on organising the supporting health system building blocks such as financing and health information systems.7
Health systems in LMICs often don’t offer an essential package of screening and treatment for T2D and HT due to limited financial resources, competing priorities and insufficient capacity. As a result, many people have limited access to adequate care and receive diagnosis and treatment late. In HICs, vulnerable populations are at increased risk of being excluded from the integrated care package.8 There is thus an urgent need to scale up integrated care for these chronic conditions and these vulnerable populations in a sustainable and effective way.
The SCUBY objectives
The SCUBY projects involves three distinctly different countries: Cambodia, Slovenia and Belgium. The countries show a range of epidemiological transitions, health systems and health policies. Furthermore, they have different resource availabilities and socioeconomic and political attributes. Rooted in their societal and health system’s context, these countries adopted distinct strategies for the integrated care package for T2D and HT.
SCUBY allows us to understand what enables the scale-up of the integrated care package for T2D and HT in different types of settings and to develop and test multiple strategies that can be adapted for replication in various healthcare systems.
The research objectives of the project are:
- To analyse the organisational capacity to scale up integrated care for T2D and HT in Belgium, Slovenia and Cambodia and to assess contextual barriers and facilitators to do so
- To develop and implement roadmaps for a national scale-up strategy in each country
- To evaluate the impact on health outcomes and quality of care through the scale-up of the integrated care package
- To generate lessons across contexts on the scale-up strategies for integrated care for T2D and HT.
Approach and methods
Scale-up is the “efforts to increase the impact of health interventions so as to benefit more people and to foster policy and programme development on a lasting basis”.9 To compare strategies across the three countries, we use the EXPAND framework to systematically document the scale-up strategy, the processes of change, the actors and the context.
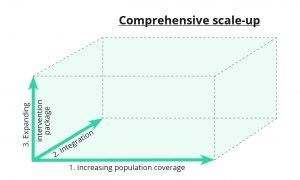
In this regard, scale-up goes beyond increasing the coverage of an intervention and must include further dimensions in order to integrate it into policy, supporting both long-term availability and sustainability. We have developed a three-dimensional framework of scale-up of the integrated care package:
- Increasing population coverage
- Expanding the intervention package
- Integration of the integrated care package into the health system.
The SCUBY project commences with an informative phase (year one), followed by an implementation phase (years two to three) and an evaluation phase (year four) (Fig. 1).
During the informative phase the integrated care package will be at the core of the research. Three sub-studies will be undertaken for:
- An in-depth analysis of implementation sites
- The effectiveness of implementation
- The mapping and analysis of the national context and stakeholder engagement.
The second and third years focus on the scale-up roadmaps and entail various steps to:
- Optimise, in co-creation with stakeholders, roadmaps and recommend key actions
for implementation - Support implementation by providing cost and monitoring information
- Evaluate the process of the scale-up roadmap implementation.
The fourth year comprises:
- Evaluation of progress along the three axes of scale-up (Fig. 1)
- Cost evaluation
- An impact evaluation.
Expected results
The project is expected to result in a set of roadmaps for a comprehensive scale-up strategy for each of the three countries. These roadmaps are potentially applicable to a wide range of similar settings to increase coverage of the integrated care package for vulnerable populations. The scale-up is expected to increase the number of well-controlled patients with T2D and HT and to reduce health inequalities.
The project will put the concept of scale-up on the agenda of the stakeholders and of governments. It will allow sharing lessons among the participating countries and considerably expands the body of knowledge regarding the art of scale-up for interventions of chronic conditions in health systems in LMICs and HICs. The context-sensitive roadmaps will enable other countries to select the best practices roadmap to the integrated care package, suitable for their specific context and current scaling-up strategy.
The three study contexts render lessons for other LMICs in these domains:
- The Cambodian case on how to implement a strategy with government support for the public health services, starting from a very limited access to HT/T2D care
- The Slovenian case on how to expand the quality and offer of care package
- The Belgian case on how to collaborate between different actors in a very diverse and pluriform healthcare context.
Who are behind SCUBY?
The research consortium comprises five research partners with strong expertise in non-communicable diseases and scale-up research:
1) Institute of Tropical Medicine Antwerp, Belgium
2) National Institute of Public Health, Cambodia
3) Community Health Center Ljubljana, Slovenia
4) University of Antwerp, Belgium
5) University Medical Center Utrecht, the Netherlands.
The project is strongly embedded in the three study countries through links with policymakers and implementation organisations.
Co-Authors
J van Olmen, Kerstin Klipstein-Grobus,3 Tonka Antonija Poplas Susicˇ,4 Ir Por,5 Edwin Wouters,2 Wim Van Damme,1 Tanja Stjepanovicˇ, Caroline Masquillier,2 Kunthea Yem,5 Daniel Boateng,3 Roy Remmen,2 Valérie Dossogne1 – on behalf of the SCUBY Consortium.6,7
- Institute of Tropical Medicine Antwerp, Belgium
- University of Antwerp, Belgium
- University of Utrecht Julius Center, Netherlands
- Community Health Center Ljubljana, Slovenia
- National Institute of Public Health, Cambodia
- The SCUBY consortium comprises the following people, in addition to the authors explicitly mentioned: Irena Makivicˇ,4 Vannarath Te,5 Monika Martens,1 Katrien Danhieux,2 Zalika Klemenc Ketis,4 Valentina Rupel Prevolnik,4 Veerle Buffel,2 Gareth White,1 and Kristien van Aerde1
- This project is funded by the Horizon 2020 programme of the European Union
References
- Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. Global burden of hypertension: analysis of worldwide data. Lancet [Internet]. 2005;365(9455):217–23. Available from: http://www.ncbi.nlm.nih.gov/
pubmed/15652604 - NCDRisC. Diabetes. Evolution of diabetes over time. Diabetes Evol [Internet]. 2016 [cited 2016 Apr 18]; Available from: http://www.ncdrisc.org/
- Mills KT, Bundy JD, Kelly TN, Reed JE, Kearney PM, Reynolds K, et al. Global disparities of hypertension prevalence and control. Circulation. 2016;134(6):441–50.
- World Health Organization. From Burden to “Best Buys”: Reducing the Economic Impact of Non-Communicable Diseases in Low- and Middle-Income Countries. Health Promotion. Geneva; 2011.
- WHO Independent High-level Commission on NCDs. Report of the technical consultation. Vol. 615. 2018.
- Package of essential noncommunicable (PEN) disease interventions for primary health care in low-resource settings WHO PEN Protocol 1 Prevention of Heart Attacks, Strokes and Kidney Disease through Integrated Management of Diabetes and Hypertension. :14–7. Available from: http://www.who.int/ncds/management/
Protocol1_HeartAttack_strokes_kidneyDisease.pdf?ua=1 - Palma AM, Rabkin M, Nuwagaba-Biribonwoha H, Bongomin P, Lukhele N, Dlamini X, et al. Can the Success of HIV Scale-Up Advance the Global Chronic NCD Agenda? Glob Heart [Internet]. 2016 [cited 2018 Mar 26];11(4):403–8. Available from: http://www.ncbi.nlm.nih.gov/pubmed/27938826
- Hecke A Van, Heinen M, Fernández‐Ortega P, Graue M, Hendriks JML, Høy B, et al. Systematic literature review on effectiveness of self‐management support interventions in patients with chronic conditions and low socio‐economic status. J Adv Nurs [Internet]. 2017;73(4):775–93. Available from: https://doi.org/10.1111/jan.13159
- Simmons R, Shiffman J. Scaling up health service innovations: a framework for action. Scaling up Health Service Delivery: From Pilot Innovations to Policies and Programmes. World Health Organization; 2007. p1-30
- Meessen B, Shroff ZC, Ir P, Bigdeli M. From Scheme to System (Part 1): Notes on Conceptual and Methodological Innovations in the Multicountry Research Program on Scaling Up Results-Based Financing in Health Systems. Heal Syst Reform [Internet]. 2017;3(2):129–36. Available from: https://www.tandfonline.com/doi/full/10.1080/
23288604.2017.1303561 - Organization WH. World Health Report, 2010: Health systems financing the path to universal coverage. World Heal Report, 2010 Heal Syst Financ path to Univers Cover [Internet]. 2010 [cited 2018 Feb 2]; Available from: https://www.cabdirect.org/cabdirect/abstract/20113042170
Josefien Van Olmen
SCUBY Project
Institute of Tropical Medicine & University of Antwerp
info@scuby.eu
www.scuby.eu
Please note, this article will appear in issue 9 of Health Europa Quarterly, which will be available to read in April 2019.








