Anders Linden on the mapping of immune signalling via the cytokine interleukin-26 to identify novel diagnostic and therapeutic targets in COPD.
In the research group of Professor Anders Lindén, the main scientific focus is set on the characterisation of immune signalling via cytokines in pulmonary host defence in health and disease, primarily with reference to the alterations among long-term (chronic) tobacco smokers that are associated with development of chronic obstructive pulmonary disease (COPD) and chronic bronchitis (CB). Professor Lindén has a long-term interest in T cell cytokines that contribute to the mobilisation of innate effector cells in the lungs. In the late 1990s, his research group published the first studies on immune signalling via the archetype T helper (Th) 17 cytokine interleukin (IL)-17 on the innate immune response in the lungs. This cytokine is now being targeted in clinical trials on asthma and COPD. During the last 10 years, Professor Lindén and his co-workers have characterised the involvement of several additional T cell cytokines in immune signalling of pulmonary host defence in chronic tobacco smokers.
More recently, Assistant Professor Karlhans Fru Che has led a new line of research on the Th17-associated cytokine IL-26 together with Professor Lindén. In a novel study, they and their co-workers now show that that the cytokine IL-26 displays high protein levels in the normal human lung, and that these levels are substantially increased among chronic smokers, with or without COPD. These IL-26 levels are further increased in chronic smokers, with or without COPD, who have CB, exacerbations of COPD, or are colonised by pathogenic bacterial species. These findings unveil novel molecular disease mechanisms in the lungs that may constitute diagnostic and therapeutic targets in chronic tobacco smokers with COPD and/or CB.
COPD
The lung disease chronic obstructive pulmonary disease is an important global cause of morbidity and mortality. Globally, COPD accounts for up to 5% of total disease-related deaths and will become the third leading cause of these deaths by 2030 according to the World Health Organization (WHO).
The major risk factor of COPD in most countries is chronic tobacco smoking. Traditionally, COPD was more common in men, but because of increased tobacco use amongst women in high-income countries as well as exposure to indoor pollution from biomass fuel used for cooking and heating in low-income countries, the distribution of COPD amongst men and women is now almost equal.
The prevalence of COPD in Europe is between 4% and 10% of adults and more than 73% of deaths due to COPD are now linked to tobacco smoking. Notably, these deaths are expected to increase from almost 270,000 in 2005 to 338,000 deaths by 2030, according to the European COPD Coalition (ECC). As a consequence, the direct cost from COPD was over €38.6 billion in 2005, representing about 3% of total healthcare expenditure in EU countries, and these costs are on the rise according to reports from the European Union (EU).
The adverse effects of chronic smoking require decades to develop before becoming clinically apparent. Therefore, despite vigorous public health campaigns against tobacco smoking and other risk factors, the clinical consequences of COPD and CB are likely to remain for several decades to come. In addition, current methods for diagnosis and therapy are insufficient. A substantial portion of patients remain undiagnosed even in developed countries and, even when diagnosed, the therapy these patients receive has limited effect on symptoms, poor effect on long-term prognosis and almost no effect on long-term survival. The one exception from this is smoking cessation; the only ‘treatment’ that has a clear proven effect in terms of long-term prognosis.
Smoking cessation remains the most effective ‘treatment’ until date. Tentatively, there is an unmet medical need for improvement of the current methods of diagnosis, monitoring, and treatment of these disorders. The members of the research group of Professor Lindén perform studies on immune signalling in tobacco-related lung disease in an attempt to meet this medical need.
Chronic bronchitis
Patients with COPD frequently suffer from chronic bronchitis (CB), a comorbidity characterised by chronic cough with mucus production. Patients with COPD and/or CB display repeated bacterial infections which cause severe worsening (exacerbations) of the disease, a higher risk for disease progression and a poor long-term prognosis. This results in high healthcare costs and acute deaths.
An important and challenging mechanistic factor in patients with these pulmonary morbidities is that these patients show high levels of neutrophils, a dedicated population of antibacterial immune cells. Neutrophils are the most abundant white blood cells in humans and constitute a very important arm of the innate immune system. Their specialised property to move towards infectious and inflammatory stimuli (chemotaxis) allows them to accumulate at sites of infection and inflammation for the sole purpose of eliminating the problem. Unfortunately, when present in excess numbers, these cells drive chronic inflammation and tissue destruction, phenomena commonly found in the lungs of chronic smokers with COPD and/or CB. It is noteworthy that although neutrophils are ‘professional killers of bacteria’, chronic smokers with COPD and/or CB with an abundance of locally accumulated neutrophils are clearly more susceptible to bacterial infections than healthy non-smokers. This paradox indicates that there is a fundamental malfunction in pulmonary host defence that we do not understand and therefore is in need of further investigation. Understanding this malfunction may provide clues to how we can develop effective therapy.
The research group of Professor Anders Lindén is now actively exploring novel aspects of immune signalling via IL-26, in particular with reference to the following aspects:
- Detection of IL-26 in human lungs;
- Mechanistic role of IL-26 in antimicrobial host defense;
- Characterisation of various cellular sources of IL-26 in the lungs;
- Release of IL-26 in response to bacterial as well as viral stimuli;
- Intracellular signalling pathways involved in the release of IL-26;
- Release of IL-26 in response to components other than endotoxin in tobacco smoke;
- Alterations of IL-26 in chronic smokers, with or without COPD, CB, and emphysema; and
- Impact of common pharmaceutical agents against COPD and CB on the production and release of IL-26 in the lungs.
Interleukin-26 belongs to the IL-10 family and this cytokine is involved in Crohn’s disease, rheumatoid arthritis, and chronic Hepatitis C virus infections. Of note, these are all chronic inflammatory disorders characterised by increased neutrophil accumulation as well. IL-26 has also been shown to be involved in antibacterial responses, with the ability to kill gram-negative bacteria through the formation of pores on the bacterial cell membrane.
Importantly, the lungs are constantly exposed to harmful particles, mists, gases, and microbial pathogens in our external environment. Consequently, the lungs are constantly under attack and at risk for bacterial or viral infections and inflammatory reactions of the immune system. Both Dr Che and Professor Lindén are optimistic about the possibility that IL-26 is a cytokine protein that is critically involved in both anti-bacterial and anti-viral host defence in the lungs and is relevant for diagnosis and therapy in pulmonary morbidities linked to excessive mobilization of neutrophils.
The involvement of IL-26 in disease mechanisms of the lungs
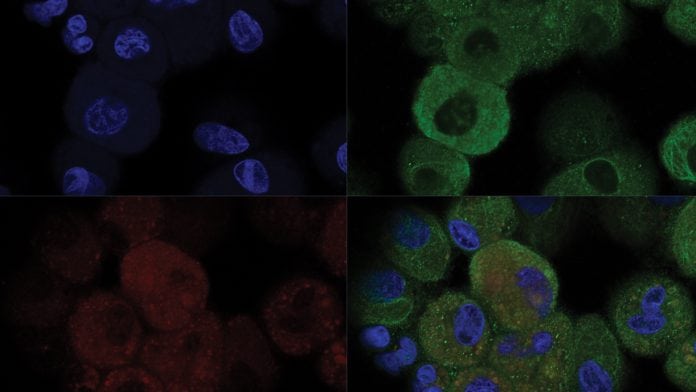
In their first study on IL-26 in the lungs, with Dr Che as lead author, Professor Lindén and his co-workers showed that the IL-26 protein is present in the lungs in bronchial segments of healthy non-smokers. Interestingly, after intra-bronchial exposure to endotoxin, a compound from gram-negative bacteria, the levels of IL-26 were substantially increased in these healthy non-smokers. This argues that IL-26 is involved in host defence against gram-negative bacteria in human lungs. Intriguingly, Professor Lindén and his co-workers showed that the Th17 cytokine IL-26 is also produced in alveolar macrophages, the most abundant immune cell in the airways.
In a separate study, again with Dr Che as the lead author, Professor Lindén and his co-workers investigated bronchial epithelial cells. These structural cells function as an important barrier in the airways, sealing the walls of the lungs against penetration of dangerous foreign substances.
Here, Professor Lindén and his co-workers revealed that among the immune functions of these cells, these cells produce IL-26 upon encounter with a viral compound called poly IC. It was also shown that that the release of IL-26 follows a pro-inflammatory pathway, involving the cell surface receptor Toll-like receptor 3, the adaptor protein TRIF, the signal transduction molecules MAP kinases, and the transcription factor NF-κB. Since bronchial epithelial cells direct viral tropism more than any other cell type in the lungs, this finding suggests that IL-26 is also involved in antiviral responses in the lungs. Moreover, the identification of the route through which this novel cytokine is released may be important in disorders that benefit from modulation of its production.
The pro- and anti-inflammatory properties of IL-26 in the lungs
When examining airway leukocytes obtained from healthy human donors through bronchoalveolar lavage, Professor Lindén and his co-workers showed that stimulation with recombinant human (rh) IL-26 protein in vitro results in an increase in the release of the pro-inflammatory mediators IL-8, IL-1β, TNF-α, and GM-CSF. In contrast, stimulation of bronchial epithelial cells with rhIL-26 inhibits the release of these same cytokines. This doubled-edged action of IL-26 suggests that IL-26 possess both pro- and anti-inflammatory responses which are determined by the specific target cell in question.
Furthermore, Professor Lindén and his co-workers showed that stimulation of neutrophils that have been isolated from healthy non-smokers with rhIL-26 alone inhibits the spontaneous migration of neutrophils (chemokinesis), whereas stimulation in the presence of the neutrophil mobiliser IL-8 potentiates the induced mobilisation of the neutrophils. In the same manner, they showed that stimulation of neutrophils with rhIL-26 in the presence of a bacterial compound fMLP (N-Formylmethionyl-leucyl-phenylalanine) potentiates the induced mobilisation of the neutrophils.
Intriguingly, these findings suggest that IL-26 possesses both stimulatory and inhibitory effects on neutrophil chemotaxis. From a teleological point of view, this implies that by stimulating receptors on neutrophils, IL-26 focuses neutrophil chemotaxis towards bacteria and accumulated immune cells, whereas, in the absence of any threat, IL-26 restrains neutrophils chemotaxis. Moreover, Professor Lindén and his co-workers showed that stimulation of blood neutrophils with rhIL-26 inhibits the release of the neutrophil activity marker myeloperoxidase (MPO). This argues that IL-26 may be useful for suppressing MPO-induced oxidative destruction of lung tissue during inflammations, but at the same time detrimental for suppressing MPO-induced killing of bacteria during infections.
Therefore, targeting IL-26 during inflammatory disorders and during infections in the lungs may have therapeutic potential. However, striking the balance between these two properties of IL-26 for the benefit of the patients will require deeper mechanistic studies.
IL-26 promotes and balances the antibacterial actions of the innate immune response
When investigating the impact of IL-26 on the innate immune response in a mouse model expressing the IL-26 receptor complex, Professor Lindén and his co-workers obtained evidence that it facilitates the innate immune response in the airways. They showed that the exposure of mice airways to the bacterial compound endotoxin, followed by stimulation of the airways with rhIL-26 protein, increases the IL-26 receptor complex signalling via STAT3 and enhances movement and accumulation of inflammatory cells into the lung tissue at an early time point and clears the same tissue from these cells at an intermediate time point, while increasing the accumulation of innate effector cells in the airway lumen at a much later time point.
In this way, during the course of 72 hours, key pro-inflammatory cytokines and proteinases are up- and down-regulated by IL-26 in an intriguing manner with a seemingly clear purpose; to enhance the accumulation of neutrophils and macrophages at the site of infection in the airways, while at the same time protecting the surrounding lung tissue from tissue-damaging effects of proteinases originating from the very same innate effector cells. Professor Lindén and his co-workers interpret these experimental findings as additional evidence that immune signalling via IL-26 bears potential as a therapeutic target in pulmonary morbidities linked to an excessive mobilisation of innate effector cells.
IL-26 in pulmonary morbidities signified by a malfunction in anti-microbial host defence
In their novel study on alterations in immune signalling via IL-26 among chronic smokers, with or without COPD, CB and colonisation by pathogenic bacterial species, Professor Lindén and his co-workers made five fundamental observations.
First, they observed that the smokers, with or without COPD, displayed increased concentrations of IL-26 protein in the lungs, in comparison to healthy non-smokers. However, they were unable to prove that the smokers with COPD differ from those without COPD during stable clinical conditions.
Second, they observed that chronic smokers with COPD displayed increased concentrations of IL-26 protein during exacerbations (a condition signifying worsening disease conditions), in comparison to stable clinical conditions in the very same subjects.
Third, they observed that smokers with or without COPD who also have CB displayed increased concentrations of IL-26 in the lungs, in comparison to those who did not have CB.
Fourth, Professor Lindén and his co-workers observed that chronic smokers with or without COPD, who had growth of pathogenic bacteria in samples from the lungs, also had increased concentrations of IL-26 in the matching lung samples, in comparison to those who did not have growth of pathogenic bacteria in the corresponding samples.
Fifth, they observed that these increase in the concentrations of IL-26 correlated with poor lung function, neutrophil mobilisation, and pro-inflammatory cytokine signalling.
Substantiating these findings, they found that stimulation of alveolar macrophages with water-soluble tobacco smoke extract in vitro, triggered increased production of IL-26 and in the same setting, stimulation with rhIL-26 triggered increased transcription of pro-inflammatory genes.
Novel findings
The novel findings on IL-26 in pulmonary host defence that are presented in this profile review position this particular cytokine protein as a promising molecular target in the lungs that can help improve the understanding of disease mechanisms characterised by chronic inflammation and repeated bacterial infections. For Professor Lindén and his co-workers, this makes IL-26 an interesting area of research, given that their overall goal is to contribute to the long-term process of improving diagnostic methods and therapy for patients with COPD and/or CB.
References
- Che KF, Tengvall S, Levanen B, Silverpil E, Smith ME, Awad M, et al. Interleukin-26 in antibacterial host defense of human lungs. Effects on neutrophil mobilization. American journal of respiratory and critical care medicine. 2014;190(9):1022-31. doi: 10.1164/rccm.201404-0689OC. PubMed PMID: 25291379.
- Tengvall S, Che KF, Linden A. Interleukin-26: An Emerging Player in Host Defense and Inflammation. Journal of innate immunity. 2016;8(1):15-22. doi: 10.1159/000434646. PubMed PMID: 26202572.
- Che KF, Kaarteenaho R, Lappi-Blanco E, Levanen B, Sun J, Wheelock A, et al. Interleukin-26 Production in Human Primary Bronchial Epithelial Cells in Response to Viral Stimulation: Modulation by Th17 cytokines. Molecular medicine. 2017;23. doi: 10.2119/molmed.2016.00064. PubMed PMID: 28853490.
- Bao A, Che KF, Bozinovski S, Ji J, Gregory JA, Kumlien Georen S, et al. Recombinant human IL-26 facilitates the innate immune response to endotoxin in the bronchoalveolar space of mice in vivo. PloS one. 2017;12(12):e0188909. doi: 10.1371/journal.pone.0188909. PubMed PMID: 29206862.
- Che KF, Tufvesson E, Tengvall S, Lappi-Blanco E, Kaarteenaho R, Levanen B, et al. The neutrophil-mobilizing cytokine interleukin-26 in the airways of long-term tobacco smokers. Clinical Science (London). 2018;132(9):959-83.
Professor Anders Lindén
Unit for Lung and Airway Research
Institute of Environmental Medicine
Karolinska Institutet
PO Box 210
SE-17177 Stockholm
Sweden
+46 8 5248 2217
anders.linden@ki.se
This is a commercial article that will appear in Health Europa Quarterly issue 6, which will be published in August, 2018.
























