In a world first, researchers have evaluated and concluded the impact of detergent-disinfectant wipes on patient outcomes, including in-hospital mortality1. GAMA Healthcare explores…
Contaminated surfaces are a problem for healthcare workers and patient safety. Around the world, infection prevention and control (IPC) workers are tirelessly crafting practices and nurturing behaviours in the hope of reducing the risk of patients contracting infections during their stay.
But what if their efforts are undermined by one simple factor… the wrong protocol?
New evidence for replacing chlorine with 2-in-1 wipes
The ultimate goal of any IPC practice is to help save lives; for the first time, researchers have endeavoured to prove just that.
When researchers from Israel’s Shamir Medical Centre replaced their traditional chlorine-based protocol with a simple 2-in-1 wipe (Clinell Universal Wipes), they demonstrated:
- Improved cleaning frequency
- Reduced room contamination
- Fewer new multi-drug resistant organism (MDRO) acquisitions
- Lower in-hospital mortality
Like many healthcare organisations, Shamir Medical Centre used a 1,000ppm chlorine solution to disinfect surfaces, along with multi-use buckets and cloths.
Effective decontamination requires 2 steps – cleaning and disinfection
Chlorine’s critical flaw is that it has no cleaning properties and is inactivated by organic matter2 – making it unsuitable for removing dirt or bodily fluids without a pre-cleaning step. An effective environmental decontamination protocol should factor in both steps required to make surfaces safe: cleaning and disinfection.
Cleaning is a vital step to achieve good decontamination as it removes physical organic matter such as dirt and bodily fluids. In the absence of matter, the disinfection step is significantly easier. This second step is focussed on killing microorganisms to reduce the infection risk associated with the surface.
It is well-recognised in peer-reviewed publications that ‘Improved cleaning and disinfection of room surfaces decreases the risk of healthcare-associated infections’3.
Effective environmental decontamination can be achieved in two separate, laborious steps or simply using a ready-to-use 2-in-1 wipe.
2-in-1 wipes achieve decontamination in 1 step
Typically, 2-in-1 wipes are formulated to include a detergent and disinfectant, which help achieve cleaning and disinfection. This study used Clinell Universal Wipes, which contain both elements and benefit from a combination of biocides which enhance their antimicrobial performance.
In the case of Shamir Medical Centre, not only would 2-in-1 wipes offer a simplified process for users, but placed in a dispenser at the patient’s bedside, the protocol would also support correct decontamination practice and improved compliance.
Tackling HCAIs with environmental decontamination
In healthcare, pathogens are a constant concern in the battle to reduce hospital infection rates. Patients are susceptible to developing infections during their stay, and contracting an HCAI is proven to increase length of stay and associated costs of care4. In fact, patients with an HCAI are estimated to cost 3 times more than those without5.
The environment plays a significant role in the transmission of pathogens in healthcare6. Each contaminated surface hosts a reservoir of infection-causing microorganisms – especially high-touch surfaces and shared patient equipment. When touched or disturbed by busy healthcare workers or patients, those pathogens are transferred via the chain of infection.
Developing effective environmental decontamination products, and ensuring they are used correctly, is key to breaking this link in the transmission of infections.
Building a breakthrough trial
From October 2016 to January 2018, 4 medical departments participated in a crossover trial. For 6-month periods, they randomly adopted one of two environmental decontamination protocols before swapping to the alternative:
- Chlorine solution (1,000ppm) plus multi-use buckets and cloths
- Clinell Universal Wipes placed bedside in a dispenser
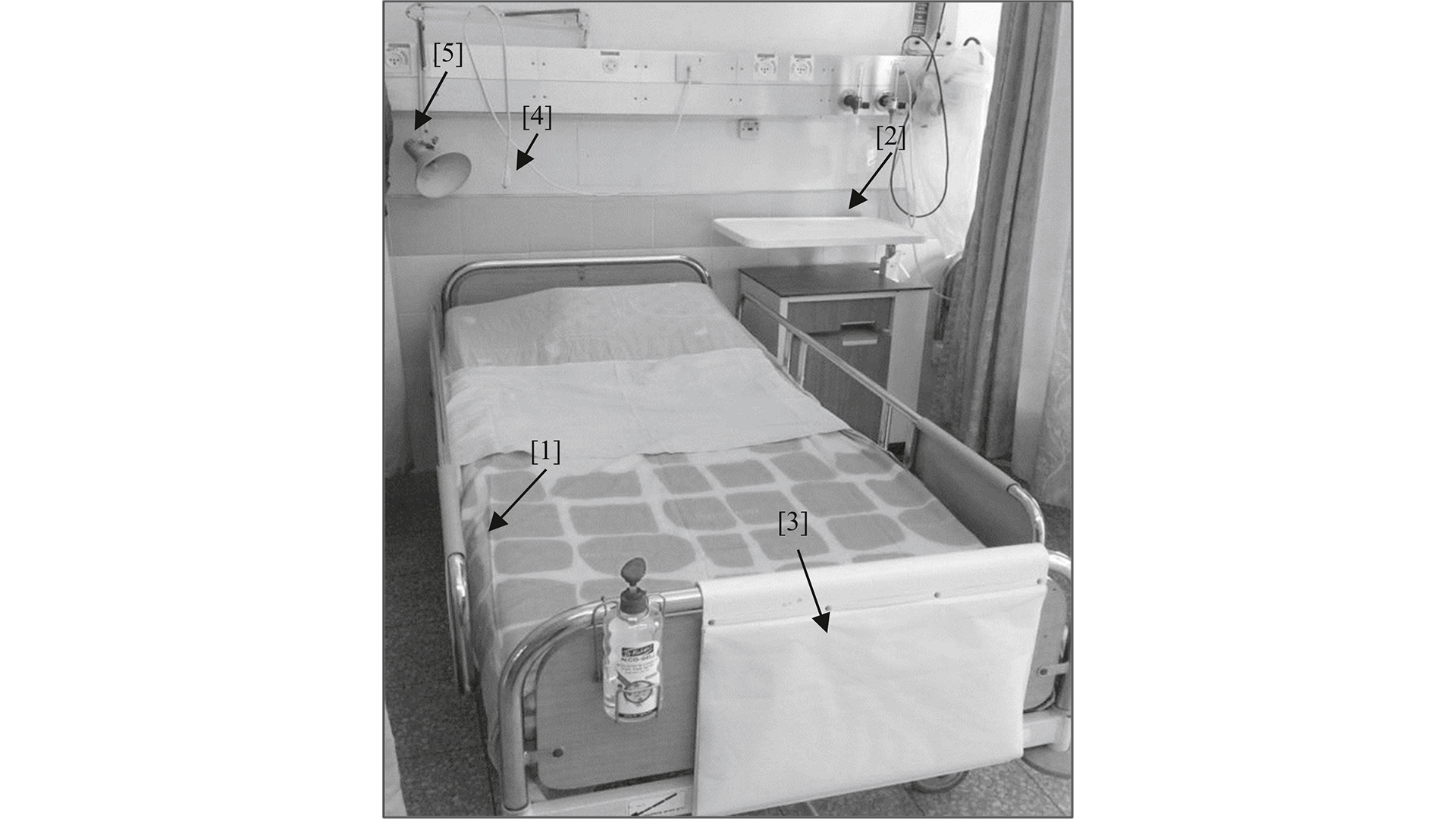
In order to quantify how effective the wipe-based protocol was, researchers looked to pull real-life data from both phases, control and intervention. They examined medical charts, undertook clinical and microbiological sampling and surveillance, and audited high-touch points with a fluorescent marker auditing kit (Clinell EvaluClean).
The fluorescent pen and torch system allowed researchers to mark and monitor cleaning performance across 5 high-touch points. If correctly decontaminated, the mark would be removed and reflected by positive cleaning frequency.
Generating real-life data
In-vitro laboratory testing can be an incredible tool for IPC teams looking at antimicrobial efficacy. Continuous advancements in microbiology and laboratory testing have opened the door to clinical performance by mimicking real-world, dirty conditions and practical contact times.
Better awareness of standardised EN testing has also helped predict and understand how antimicrobial formulations behave when applied to various test microorganisms. However, there is a growing need to see these test results reflected in evidence gained from real-world clinical settings.
In combination, laboratory testing and peer-reviewed clinical evidence build a complete picture that demonstrates how effective a product truly is at wiping out infections.
Emerging results
The enormity of this ‘large, ‘real-world’ interventional study’ is note-worthy. For the team of researchers at Shamir Medical Centre, the quest to generate data encompassing different measures of successful environmental decontamination pulled information from 7,725 patients and 46,670 patient-days.
They added: “The study was executed on crowded governmental Medicine floors with multi-patient rooms. By simply placing cleaning/disinfecting wipes in patients’ immediate environment, we have been able to generate controlled estimates for the impact of improved cleaning on patient outcomes.”
Placing wipes at patients’ bedside promotes good practice
In real-world healthcare settings, multi-patient wards are full of life. Healthcare workers are challenged with juggling patient care and high standards of environmental decontamination.
Using a 2-in-1 wipe immediately eliminates the need for more than one product, meaning everything needed to decontaminate equipment is readily available. No need to collect products, no dilutions, no cumbersome cloths and buckets, no waiting for drying in between cleaning and disinfection steps. Simply remove a wipe and complete the task at hand.
As well as a simple product, strategic placement helps ensure that decontamination is undertaken at the moment that matters.
Dispensers make the difference
Placed in a dispenser at the point of use, wipes are easily accessible to busy healthcare workers. In this study, dispensers were placed at patients’ bedside in multi-bed patient rooms.
In the direct eye line of busy healthcare workers, the dispenser acts as a visual reminder and removes the time taken to locate multiple products.
“We noticed the importance of locating the wipes in a hanger that is connected to the wall at the patient’s unit… it is easily noticed when the hanger is empty, so that missing wipes should be replaced.”
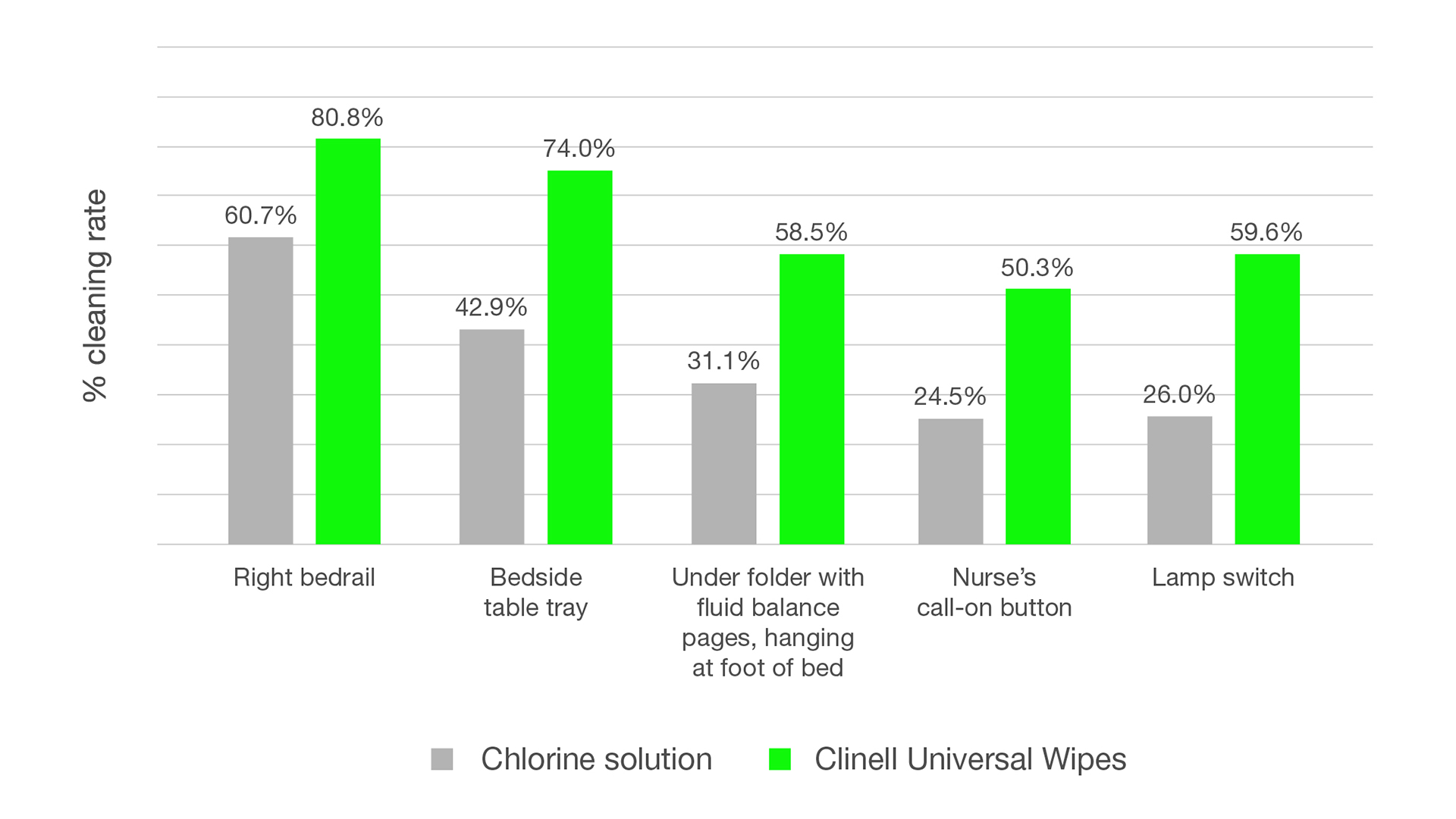
Results showed that placing wipes at patients’ besides improved environmental cleaning frequency by 33.6%. In some instances, the frequency of cleaning nearly doubled with the implementation of the Clinell Universal Wipe and dispenser protocol.
Training to support compliance
To support implementation, healthcare workers received training to support correct use of Clinell Universal Wipes and dispensers. Training and education are imperative to successfully implementing any new process and go hand in hand with a simplified protocol in improving compliance with IPC initiatives.
A study conducted in Scotland showed that introducing Clinell’s 2-in-1 coupled with GAMA Healthcare‘s advanced training programme halved the time taken to decontaminate common pieces of equipment7. The study goes on to conclude that ‘The assumption that all nurses know how to clean is erroneous’.
Before the intervention, Lanarkshire were using a chlorine-based protocol comprising a detergent followed by a sodium hypochlorite solution – a laborious and time-consuming protocol similar to that used by Shamir Medical Centre pre-intervention.
By providing enhanced training and education, with the support of well-placed dispensers, the IPC Team at NHS Lanarkshire implored to ‘make it easy for healthcare workers to do the right thing’.
For researchers at Shamir Medical Centre their results mirrored these findings. They also acknowledged the importance of dispensers and observed improvements in decontamination results, this time in reference to compliance with cleaning frequency and reduction in MDRO room contamination.
Wipes impact patient safety
The study observed the acquisition rates of MDROs within each ward, looking specifically at the most epidemiologically significant human pathogens, including MRSA, VRE, CRE, A.baumannii, and P. aeruginosa.
Across each pathogen, the Clinell protocol was found to reduce MDRO acquisition rates. This observation aligns with other findings, which have shown significant reductions in other significant pathogen acquisitions, such as a 55% reduction in MRSA documented by Garvey et al in the Journal of Hospital infection8.
Importantly, this new study is the first to measure and conclude the impact of wipes on patient survival. For the first time, the implementation of Clinell Universal Wipes has been proven to contribute towards improved in-hospital mortality rates as part of a holistic environmental decontamination strategy. This finding demonstrates the positive impact of introducing a simple and time-saving7 protocol on patient outcomes.
Consider a simplified protocol
Reflecting on this ground-breaking study, there is sufficient evidence to support the use of detergent-disinfectant wipes in place of chlorine solutions. Replacing chlorine solutions with Clinell Universal Wipes and dispensers:
- Improves cleaning and disinfection of high-touch points
- Reduces environmental contamination
- Reduces pathogen acquisition
- Improves outcomes in healthcare
Researchers concluded: ‘This is a feasible, recommended practice to improve patient outcomes in multi-patient rooms’.
As Infection Prevention and Control Teams strive to improve patient care, this simple, practical solution could be the key to unlocking their success.
Contact Gama Healthcare here to find the best infection prevention solutions for you.
References
- Dadon M, Chedid K, Martin ET, et al. The impact of bedside wipes in multi-patient rooms: a prospective, crossover trial evaluating infections and survival. J Hosp Infect. 2023;134:50-56. doi:10.1016/j.jhin.2022.11.025
- Rutala WA, Weber DJ. Uses of inorganic hypochlorite (bleach) in health-care facilities. Clin Microbiol Rev. 1997;10(4):597-610. doi:10.1128/CMR.10.4.597
- Weber DJ, Anderson D, Rutala WA. The role of the surface environment in healthcare-associated infections. Curr Opin Infect Dis. 2013;26(4):338-344. doi:10.1097/QCO.0b013e3283630f04
- Manoukian S, Stewart S, Dancer S, et al. Estimating excess length of stay due to healthcare-associated infections: a systematic review and meta-analysis of statistical methodology. J Hosp Infect. 2018;100(2):222-235. doi:10.1016/j.jhin.2018.06.003
- The Kings Fund. Healthcare-Associated Infections: Stemming the Rise of Superbug.; 2008.
- Weber DJ, Anderson D, Rutala WA. The role of the surface environment in healthcare-associated infections. Curr Opin Infect Dis. 2013;26(4):338-344. doi:10.1097/QCO.0b013e3283630f04
- Shepherd E, Leitch A, Curran E. A quality improvement project to standardise decontamination procedures in a single NHS board in Scotland. J Infect Prev. 2020;21(6):241-246. doi:10.1177/1757177420947477
- Garvey MI, Wilkinson MAC, Bradley CW, Holden KL, Holden E. Wiping out MRSA: effect of introducing a universal disinfection wipe in a large UK teaching hospital. Antimicrob Resist Infect Control. 2018;7(1):155. doi:10.1186/s13756-018-0445-7

























