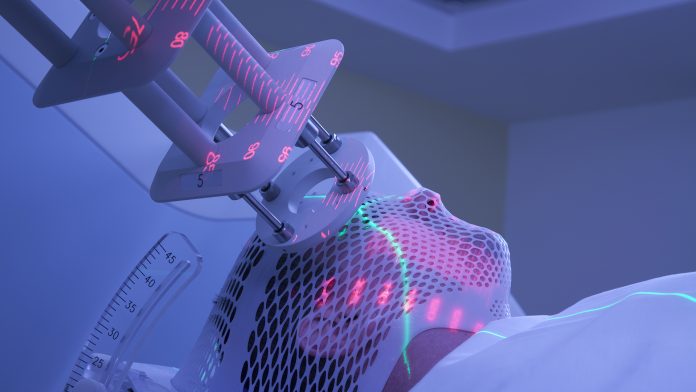
The implementation of light therapy potentially increases skin healing from damage caused by cancer radiation therapy by up to 50%.
In a new study pioneered at the University of Buffalo, researchers have identified that photobiomodulation, a type of lose-dose light therapy, mitigated the severity of skin damage from radionecrosis, which is the breakdown of the skin caused by radiation therapy. Light therapy reduced inflammation, improved blood flow, and increased wound healing for 19 days following radiation therapy.
The investigation was led by Rodrigo Mosca, PhD, a visiting fellow from the Nuclear and Energy Research Institute (IPEN) and the Federal University of Rio de Janeiro. It builds on prior studies that elucidated the effectiveness of light therapy for improving the healing of burn wounds and reducing pain from oral mucositis incurred by radiation and chemotherapy.
Senior author Praveen Arany, DDS, PhD, assistant professor of oral biology in the UB School of Dental Medicine, said: “To our knowledge, this is the first report on the successful use of photobiomodulation therapy for brachytherapy. The results from this study support the progression to controlled human clinical studies to utilise this innovative therapy in managing the side effects from radiation cancer treatments.”
The study’s findings are published in Photonics.
Brachytherapy damage
Brachytherapy is a type of radiation therapy in which a source of radiation is embedded within the cancer tissue, subsequently exposing the surrounding healthy tissue to a lower dose of radiation than teletherapy – where beams of radiation are fired through the skin to attack the tumour. However, despite brachytherapy being more accurate and safer than alternative cancer treatments, skin damage is still caused during the process.
Employing light therapy
Earlier research from the team signified that light therapy promotes healing through activating a protein that regulates cell growth and division – called TGF‐beta 1 – by stimulating cells involved in healing, including fibroblasts and macrophages. Fibroblasts are the primary connective tissue cells of the body that are essential in tissue repair, whereas macrophages are immune cells that lower inflammation, clean cell debris, and fight infection.
For their study, the team, using an animal model, tested the effectiveness of near-infrared and red LED light at improving skin healing during radiation therapy. Without light therapy, it took an average of 61 days for wounds to heal. Near-infrared light therapy took an average of 49 days to heal wounds, with red light therapy being the fastest at an average of 42 days.
Mosca commented: “For over 40 years, photobiomodulation has been known to accelerate the healing of acute and chronic wounds, triggering cellular processes that control inflammation, pain signalling, and tissue regeneration and repair.”
“Research suggests that the effects of photobiomodulation do not extend to tumour cells, likely due to their perturbed metabolic and regulatory signalling,” added Arany.