Scientists in China have developed an automated system that expertly pinpoints the best antibiotics for treating blood infections, a potentially life-saving innovation that will help to reduce antimicrobial resistance (AMR).
It is essential for healthcare professionals to rapidly and accurately identify the most optimal antibiotics for fighting blood infections to achieve the best patient outcomes. To enhance this process, researchers from the Qingdao Institute of Bioenergy and Bioprocess Technology (QIBEBT) of the Chinese Academy of Sciences (CAS) and Peking Union Medical College Hospital have developed an automated system that provides efficient results for determining the best antibiotics at the correct dose.
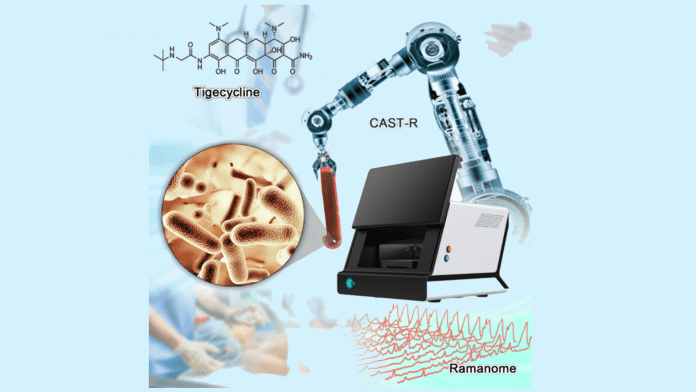
The novel system, which is called the Clinical Antimicrobials Susceptibility Test Ramanometry (CAST-R), is based on Raman microspectroscopy, a type of spectroscopic method that can isolate specific molecules. The cutting-edge device will potentially enhance the treatment of blood infections and reduce the burden of AMR.
Limitations of current techniques
Antimicrobial susceptibility tests (ASTs) are the standard method for determining antibiotics best suited for combatting a particular bacteria or fungus; however, they are time-consuming, labour intensive, and unstable.
For acute blood infections such as sepsis – which has a mortality rate between 20% and 40% – each hour’s delay in attaining an AST report increases the mortality rate by 7.6%. Tigecycline is the last-resort antimicrobial that is employed to treat blood infections.
YANG Qiwen, the senior author of the study and Associate Director of the Department of Clinical Laboratory, Peking Union Medical College Hospital, commented: “Unfortunately, resistance to tigecycline has emerged in many blood pathogens.”
A drawback of currently used ASTs for tigecycline is that they are slow, inefficient and have low accuracy. Moreover, the AST of tigecycline takes between 36 and 48 hours to complete.
“Rapid and reliable methods for tigecycline resistance are urgent,” said ZHU Pengfei, a scientist with QIBEBT, CAS.
Enhancing care for blood infections
The team’s CAST-R system employs a liquid robot for sample pretreatment and a machine-learning control scheme for obtaining the data and maintaining quality control. Every Single-Cell Raman Spectrum (SCRS) produced by the technology contained thousands of Raman peaks that provide detailed information about cells.
In their study, the three-hour CAST-R process accomplished highly accurate results and was demonstrated to be ten times faster than the traditional AST method. CAST-R handled 96 paralleled antibiotic-exposure reactions and produced Raman spectra comparable to the more time-consuming manual process.
“The automation, speed, reliability, and broad applicability suggest CAST-R as a clinically valuable AST for blood infections,” said REN Lihui, an associate professor at the QIBEBT, CAS.
XU Jian, another senior author of the study and Director of Single-Cell Center at QIBEBT, commented: “The strengths of an SCRS, which also include information richness, single-cell resolution, and ability to couple with downstream single-cell sequencing, have yet to be fully exploited in this study, and that will be our priority ahead.”
The team is now working to improve the CAST-R system further.
“As we refine the CAST-R workflow process, our goal is to provide a series of new applications in clinical diagnosis based on microbial single-cell technologies in order to combat superbugs and support personalised treatment of infections,” concluded YANG Qiwen.
























