
Inflammatix explores the unmet needs associated with the diagnosis of acute infection and sepsis and how new diagnostic technologies are helping to improve the standard of care.
AMR is a leading cause of death worldwide, as stated in the recent Global Research on Antimicrobial resistance (GRAM) report1, this growing threat presents a major challenge in the treatment of sepsis.
Antimicrobial stewardship programmes (AMS) aim to improve antibiotic prescribing and can help clinicians improve clinical outcomes and minimise harm, such as adverse effects and selection for antibiotic resistance.
However, sepsis and AMS programmes coexist in tension as they can appear to have opposing messages around antimicrobial prescribing. Sepsis is a clinical diagnosis and delay to first-dose antimicrobial therapy is associated with increased mortality. However, current diagnostic tools are not very effective in discriminating between bacterial and viral infections or a systemic inflammatory response. Clinicians must therefore make a treatment decision empirically without having objective and complete information. Equally, de-escalation and cessation are hard to manage once therapy has begun, meaning patients can remain on antibiotics long after the true cause of the complaint has been established.
New point-of-care diagnostic technologies enabling real-time discrimination between infection and a systemic inflammatory response, and between bacterial from viral infections in patients with suspected acute infection and sepsis, will be crucial to reducing diagnostic uncertainty. They can help physicians avoid partially empirical prescribing decisions that can be prone to bias and aid in decreasing the overuse of antibiotics in patients suspected of acute infection and sepsis.
Amongst these new diagnostic technologies for acute infection and sepsis are host or immune response-based diagnostics, a rapidly evolving field that focuses on reading the immune response to infection. This has the potential to advance the standard of care for acute infection and sepsis, support AMS programmes, and combat AMR.
We interviewed Dr Larissa May, Professor of Emergency Medicine, and Director of Emergency Department Antibiotic Stewardship at the University of California Davis Health and a paid consultant for Inflammatix.
We know that diagnosing infection in the ED has always been challenging, is there anything new on the horizon that will really change this?
LM: The biggest challenge with the diagnostic tools available in acute care settings is that we do not currently have rapid and accurate tools to tell us the cause of suspected sepsis. We need rapid POC tests that can impact our clinical decision making. They need to be sensitive and specific if we are using them for screening of sepsis, with a very high negative predictive value (NPV). We are also missing the host response component that can help discriminate between the various types of etiologies that can cause a clinical picture that looks like sepsis. While certainly in the case of bacterial sepsis early appropriate targeted antibiotics are lifesaving, lots of broad spectrum unnecessary antibiotic use leads to adverse patient events and potentially precludes the diagnosis of what is causing the patient’s clinical picture, so having a host response test that looks at the patient’s response to infection and distinguishes between viral and bacterial or other causes of sepsis like inflammatory syndrome would be a game changer.
Do you think that host or immune response-based point-of-care (POC) tests for acute infection and sepsis could help slow the spread of AMR?
LM: Yes, implementation of these tests as part of AMS efforts paired with digital solutions and behaviour change methods could absolutely help, not only reducing patient adverse events related to excessive antibiotic use, but also slowing the downstream emergence and acceleration of AMR. The immune response approach along with the test being run at the POC with a fast test Turn Around Time (TAT) will help distinguish between bacterial and viral infection and other causes. These factors could reduce not only initiating of antibiotics for presumed viral infection but broad-spectrum empiric therapy and overall duration of antibiotics, factors known to contribute to AMR.
Where on the patient’s pathway would you use host or immune based POC testing?
LM: If a test takes a comprehensive approach to the immune response to infection, can discriminate between bacterial and viral infection, and infection and inflammation with high accuracy, it may help reduce the over-treatment of patients with suspected infection thus supporting AMS programmes.
I think they could be used first as screening tools ahead of giving antibiotics for patients who meet the clinical picture of sepsis or patients in whom a blood culture is being considered or who have markers consistent with possible sepsis such as elevated white blood cell count or lactate. Particularly patients that are on the edge of being admitted, like a wait and see approach, and for the ones that are sick enough to be hospitalised to de-escalate quickly. Given that our current biomarkers, including lactate and procalcitonin, are limited in their ability to predict bacterial infection, I see these technologies as completely replacing our current laboratory tests for screening. These technologies may also have a role in prognosis and could potentially impact patient disposition as well.
Ideally, we would love to see these tests impact that first dose of antibiotics, even if that takes some time to impact prescribing behaviour.
What are your thoughts on the existing acute infection and sepsis tests and Inflammatix approach to measure the host-immune response to infection?
LM: I think that the technology and the inclusion of machine learning can really help guide clinical decision making. The host-immune response approach is different from current biomarkers, as the diagnostic test can help discriminate between inflammation and infection in surgical patients for example, where with current tests like PCT it can be very challenging. I like the simplicity approach to results interpretation that is being developed at Inflammatix, because a lot of time new tests are difficult for us clinicians on the front line to interpret.
I also think that a POC immune response test could be useful with other clinical parameters and may help clinicians adjust their pre-test probability to guide whether the patient warrants antibiotics or broad-spectrum antibiotics or even impacting whether they think the patient should be going to the ICU based on the severity result or prognosis.
About Inflammatix
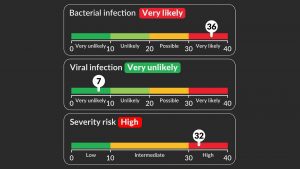
At Inflammatix, we are working to support AMS programmes and combat AMR by developing an innovative point-of-care (POC) instrument to be used with a rapid (<30-minute) whole-blood POC test to aid in the diagnosis of acute infection and sepsis.2,3 We have derived specific gene signatures associated with the immune response to infection to inform the clinician about the likelihood of bacterial and viral infection, as well as the need for ICU level care (severity). Recent publications have demonstrated its potential for improving patient care in the Emergency Department and critical care.4,5,6 Our tests have not been cleared or approved by the FDA, nor have they been CE or UKCA Marked.
References
- Murray et al, The Lancet, 2022
- Ducharme et al, Journal of Personalized Medicine, 2020
- He et al, Journal of Personalized Medicine 2021
- Safarika et al, ICMx, 2021
- Bauer et al, Bauer et al, Critical Care Medicine, 2021
- Brakenridge et al, CCx, 2021
MKT202203002REV0
This article is from issue 21 of Health Europa Quarterly. Click here to get your free subscription today.

























